-
PDF
- Split View
-
Views
-
Cite
Cite
Hideki Katagiri, Yasuo Yoshinaga, Yukihiro Kanda, Ken Mizokami, Emphysematous cholecystitis successfully treated by laparoscopic surgery, Journal of Surgical Case Reports, Volume 2014, Issue 4, April 2014, rju027, https://doi.org/10.1093/jscr/rju027
Close - Share Icon Share
Abstract
Emphysematous cholecystitis (EC) is an uncommon variant of acute cholecystitis, which is caused by secondary infection of the gallbladder wall with gas-forming organisms. The mortality rate of EC is still as high as 25%. Emergency surgical intervention is indicated. Open cholecystectomy has been traditionally accepted as a standard treatment for EC. We present a case of EC successfully treated by laparoscopic surgery. Laparoscopic cholecystectomy for EC is considered to be safe and effective when indicated.
INTRODUCTION
Emphysematous cholecystitis (EC) is an uncommon variant of acute cholecystitis, which is caused by secondary infection of the gallbladder wall with gas-forming organisms [1–5]. The mortality rate of EC is as high as 25% because of its high complication rate [2, 5] due to gangrene, gallbladder perforation, pericholecystic abscess and bile peritonitis. Emergency surgical intervention is necessary for EC treatment for which open cholecystectomy has traditionally been performed [1, 3–5]. Here we present a case of EC successfully treated by laparoscopic surgery.
CASE REPORT
A 78-year-old male was admitted to our hospital for an investigation of vertigo. He had past medical history of diabetes mellitus, hypertension and dyslipidemia. After admission, he developed fever and abdominal distention. A chest X-ray in the up-right position and abdominal computed tomography (CT) were performed. The chest X-ray showed the presence of gas within the gallbladder and in its wall (Fig. 1). The CT scan revealed emphysematous changes in the gallbladder wall and air within the gallbladder (Fig. 2A and B). Therefore, a diagnosis of EC was made. The patient was referred to the Department of Surgery and emergent surgery was performed.
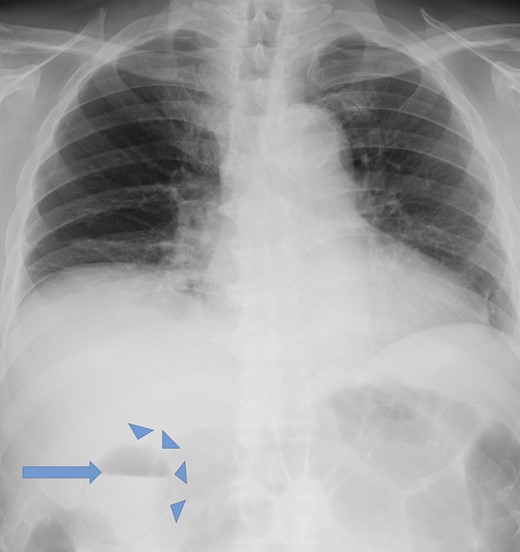
Up-right chest X-ray demonstrating air in the gallbladder (arrow) and in its wall (arrowheads).
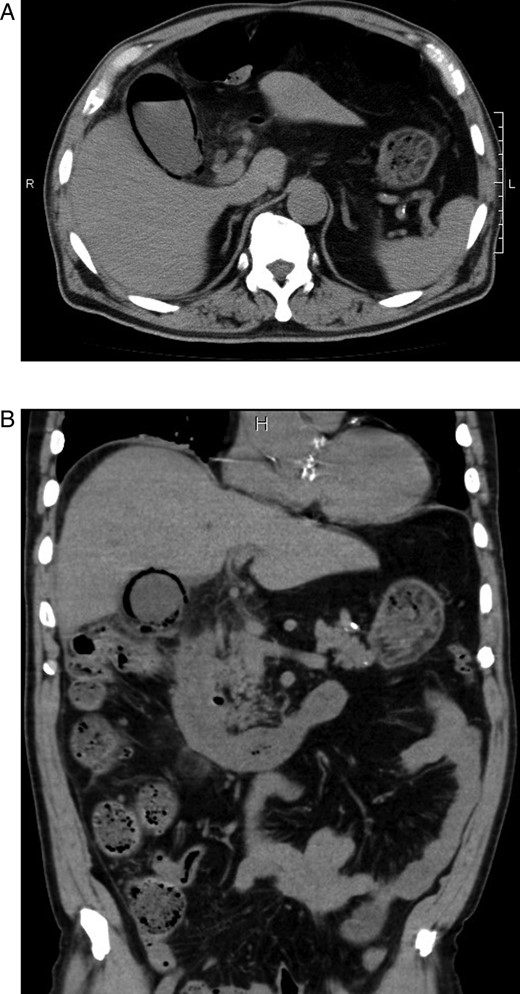
(A and B) Abdominal computed tomographic scans of axial and coronal views revealing emphysematous changes in the gallbladder wall and air in the gallbladder.
Based on the hemodynamically stable status of the patient, we selected a laparoscopic approach. Exploration of the abdominal cavity revealed gangrene and necrosis of the gallbladder. To facilitate the resection, we initially punctured the gallbladder using a percutaneous needle to extract bile. Ascites surrounding the gallbladder suggested perforation. Although there was significant adhesion, we were able to safely dissect the Calot's triangle and detected a cystic duct and artery. Gallbladder resection was successfully completed without conversion to open laparotomy. His postoperative course was uneventful. A bile culture obtained during surgery revealed Clostridium perfringens, Enterobacter cloacae and Enterococcus faecalis as the causative organisms.
DISCUSSION
EC is an uncommon variant of acute cholecystitis characterized by potentially high mortality and morbidity because of a high incidence of gangrene or perforation. Garcia et al. [2] reviewed 20 cases of EC and reported that the mortality rate was as high as 25% and the morbidity rate as high as 50%. Emergent surgical intervention for EC is indicated with cholecystectomy as the definitive treatment, although percutaneous cholecystostomy for critically ill patients presents another option [1, 4, 5]. Bouras et al. [3] reported that the laparoscopic approach for EC can be considered a safe procedure. Owing to the advances of laparoscopic surgery, it has allowed to perform emergency cholecystectomy. Our patient was hemodynamically stable; therefore, we selected the laparoscopic approach, which was successfully and safely completed. The postoperative course was uneventful.
The causative organisms of EC include C. perfringens, Escherichia coli and species of the genera Staphylococcus, Streptococcus, Pseudomonas and Klebsiella [1–5]. EC is associated with diabetes mellitus and primarily affects males, as in the present case.
The symptoms of EC are almost the same as those of acute cholecystitis, including right upper quadrant pain, nausea, vomiting and low-grade fever [2, 4]. A prompt diagnosis of EC is essential and plain abdominal X-rays or ultrasound can be diagnostically useful with a sensitivity of up to 95% [2]. However, contrast-enhanced abdominal CT scans may offer more information [1]. In our patient, a chest X-ray in the up-right position detected air in the gallbladder wall and an abdominal CT revealed typical presentation of EC.
EC is a rare but potentially life-threatening variant of acute cholecystitis. Emergency intervention is indicated and the laparoscopic approach can be considered a safe and effective method in hemodynamically stable patients.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
ACKNOWLEDGEMENTS
None.



