-
PDF
- Split View
-
Views
-
Cite
Cite
Amad Khan, Kathyrn Ellen Flavin, Lauren Sarah Harris, Mohammad Naushad Chaudhry, Nicholas Reading, Bowel hath no fury like a gallbladder inflamed, Journal of Surgical Case Reports, Volume 2014, Issue 4, April 2014, rju028, https://doi.org/10.1093/jscr/rju028
Close - Share Icon Share
Abstract
Gallstone ileus is a well-established phenomenon in which a large gallstone leads to mechanical small bowel obstruction. This case, however, reports the novel finding of a patient presenting with suprapubic pain and guarding caused by paralytic ileus of the small bowel and a duodenal perforation secondary to a necrotic gallbladder. It highlights the importance of distinguishing between gallstone ileus and paralytic ileus and how the management of the two conditions differs. Furthermore, this article discusses how paralytic ileus caused by intra-abdominal inflammatory conditions such as cholecystitis can mask the typical clinical findings making the diagnosis difficult.
INTRODUCTION
The most common cause of small bowel obstruction is adhesions post-surgery [1]—it is not known to be caused by inflammation of the gallbladder. Another surgical condition, namely duodenal perforation is associated with long-standing peptic ulcer disease [2]. While gallstone ileus is a well-established phenomenon in which a large gallstone leads to mechanical small bowel obstruction [1], this case reports the novel finding of a patient presenting with suprapubic pain and guarding caused by paralytic ileus of the small bowel and a duodenal perforation secondary to a necrotic gallbladder.
CASE REPORT
A 73-year-old male, Mr B presented to the A&E at Whipps Cross Hospital, London with a 3-day history of suprapubic pain. It was associated with some abdominal distension and bloating, and had no aggravating or relieving factors. Additionally, Mr B reported three episodes of non-projectile, non-bilious and blood-free vomiting. He had not opened his bowels for the past 5 days, but had been passing flatus. He denied any urinary symptoms, weight loss or change in bowel habit, prior to this acute episode. He was otherwise fit and healthy, had no previous surgeries and was on no medication. On examination, he was vitally stable but appeared to be dehydrated. He was tender and had guarding in the suprapubic region. He also had increased bowel sounds and was excessively tympanic on percussion of the abdomen. An inguinal hernia on the left side was noted but was reducible and non-tender.
His blood on admission showed a raised white cell count of 12.5 × 103 cells/ml (with neutrophilia) and a C-reactive protein of 14.0 mg/l. His alanine transaminase was mildly raised at 79 U/l; however, his remaining liver and renal function tests were normal. His abdominal X-ray showed dilated loops of small bowel but no evidence of large bowel dilatation (Fig. 1). A provisional diagnosis of small bowel obstruction was made and a computerised tomography (CT) scan of the abdomen and pelvis was ordered. The CT showed multiple dilated loops of small bowel but no focus of obstruction (Fig. 2a). The gallbladder wall was thickened and oedematous and there was also evidence of gas within its lumen. Air was seen under the left lobe of the liver, suggestive of a bowel perforation. Furthermore, in Fig. 2b, the second part of the duodenum appears to be adherent and in communication to the gallbladder. Putting all these findings together, the radiologist felt that there was acute cholecystitis leading to a duodenal perforation and paralytic ileus.

Plain film of the chest and abdomen: the chest X-ray shows features suggestive of air under the diaphragm, while the abdominal film shows dilated loops of small and large bowel with air in the rectum, highly suggestive of ileus.
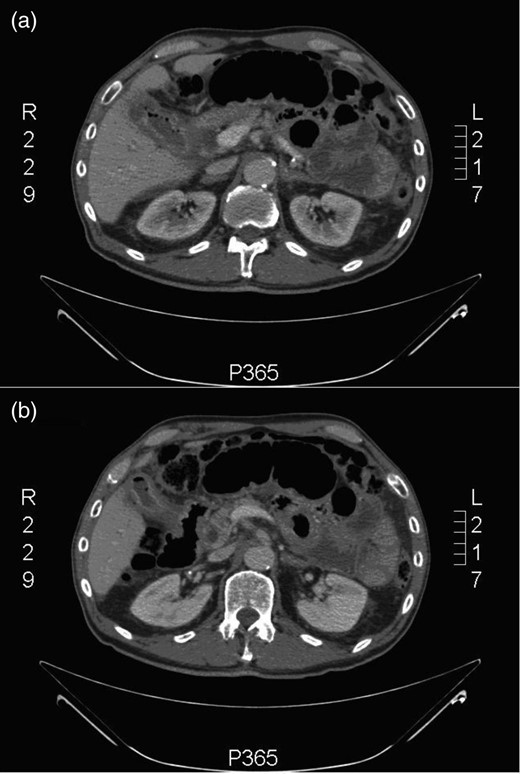
CT abdomen + pelvis: (a) inflammation of the gallbladder and (b) a very closely adherent gallbladder to the second part of the duodenum (D2).
A plan for a laparotomy was made and the patient was taken to theatre. Intra-operatively, the entire small bowel up to the ileocaecal valve was dilated with no evidence of mechanical obstruction.
The colon was dilated up to the hepatic flexure; from there onwards it was progressively collapsed. The hepatic flexure of the colon was adherent to a chronically inflamed and necrotic gallbladder. The gallbladder was friable and adherent to the first part of the duodenum. A subtotal cholecystectomy was performed due to the multiple adhesions of the gallbladder and when perforated and removed, multiple cholesterol gallstones were released. The cholecystitis had eroded a small perforation into the first part of the duodenum as well, which was repaired with an omental patch. The abdomen was washed out and a Robinson's drain left in situ. The patient recovered uneventfully and was discharged on the seventh post-operative day. The results of the histopathology of the gallbladder revealed inflammation and no malignant cells.
DISCUSSION
An interesting and rare but relevant cause of mechanical small bowel obstruction is gallstone ileus. A misnomer, for it is not a paralytic, but a mechanical obstruction caused by impaction of one or more gallstones, which have to be at least 25 mm in diameter to achieve this [3]. A fistula develops between a gangrenous gallbladder and the duodenum or other parts of the gastrointestinal tract, allowing passage of the stone [3]. The most common site of impaction of gallstones is in the distal ileum [4]. In our case, there was no fistula present but rather a duodenal perforation with free air in the abdomen as well as obstruction present to the hepatic flexure of the large bowel, ruling out gallstone ileus. The important distinction between gallstone ileus and paralytic ileus was crucial and the crux of this report: recognition of the fact that the bowel obstruction was due to paralytic ileus and not an impacted gallstone meant that a small bowel enterotomy to look for and remove an offending gallstone was not needed. The authors here hence suggest a careful review of abdominal CT images in conjunction with the radiologists pre-operatively as well as diligent inspection of small and large bowel intra-operatively in cases where there is a possibility of gallstone ileus.
There are clinical reports in the literature of peritonitis, both local and generalized, caused by acute appendicitis rarely leading to ileus [5]. The clinical features of ileus may dominate the clinical picture and mask appendicitis making the diagnosis difficult, especially in elderly patients as it did in our case: on examination, the patient was tender suprapubically rather than the right upper quadrant or epigastrium as would be expected with gallbladder inflammation. The adynamic ileus is thought to be caused by the inflammation of the appendix causing the muscles of the small bowel to be stunned into paralysis—this type of obstruction can be with or without peritonitis [6]. Since no such reports in the literature were found of gallbladder inflammation causing ileus, we hypothesize that the same inflammatory processes proposed by Harris and Rudolf [6] and Assenza et al. [5] mentioned above are responsible for the paralytic ileus seen in our case.
In conclusion, in cases where gallstone ileus is suspected, it is imperative to consider and exclude the possibility of acute cholecystitis causing paralytic ileus. Furthermore, paralytic ileus caused by intra-abdominal inflammatory conditions such as cholecystitis can mask the typical clinical findings making the diagnosis difficult.



