-
PDF
- Split View
-
Views
-
Cite
Cite
Ian C. Coulter, Sajedha Mahmood, David Scoones, Nicholas Bradey, Philip J. Kane, Abscess formation within a Rathke's cleft cyst, Journal of Surgical Case Reports, Volume 2014, Issue 11, November 2014, rju105, https://doi.org/10.1093/jscr/rju105
Close - Share Icon Share
Abstract
We report and discuss the rare case of a pituitary abscess forming within a Rathke's cleft cyst (RCC). A 66-year-old gentleman presented with visual deterioration and symptoms suggestive of hypopituitarism. The patient underwent transsphenoidal debulking of the lesion whereupon purulent material was discovered. Histological examination was suggestive of RCC together with numerous neutrophils characteristic of abscess. Microbiological culture of the material grew Staphylococcus aureus. The patient was treated for a RCC abscess and received antibiotics and endocrine replacement therapy. The patient has been followed up for 2 years without recurrence. Although uncommon, we recommend the consideration of RCC abscess as a differential diagnosis of a pituitary mass lesion as clinical presentation and radiological assessment are not specific in identifying these lesions preoperatively.
INTRODUCTION
Infection and abscess of the pituitary gland is an uncommon pathology representing <1% of all pituitary disease [1]. The majority of pituitary abscesses tend to occur in the context of a previously healthy gland, although pre-existing pituitary growths such as adenomas, craniopharyngiomas and Rathke's cleft cysts (RCCs) are thought to represent a more favourable medium for infection, so-called primary and secondary pituitary abscesses, respectively [2]. Below we present a case of abscess forming within a RCC presenting with visual impairment and hypopituitarism.
CASE REPORT
A 66-year-old gentleman presented with gradual visual deterioration, fatigue, dry skin, diminution of libido and erectile dysfunction. His past medical history was unremarkable. On examination, he appeared hypogonadal with bilateral gynaecomastia, central adiposity and diminished chest and axillary hair. He was apyrexial and appeared otherwise systemically well. A left upper quadrantonopsia was elicited on confrontation assessment of visual fields and confirmed on Goldmann perimetry.
Endocrine biochemistry was indicative of hypopituitarism [cortisol 90 nmol/l, thyroid-stimulating hormone 1.22 mU/l (T4 6.7 pmol/l), testosterone <0.4 nmol/l]. Magnetic resonance imaging (MRI) revealed a cystic sellar lesion compressing the optic chiasm (Fig. 1). Computed tomography scanning demonstrated an uncalcified hypodense cystic lesion within the sellar. Based on the radiological appearances, a macroadenoma or craniopharyngioma was suspected. A transsphenoidal decompression was undertaken whereupon yellow pus was encountered within a predominantly cystic sellar mass. The atypical appearance of the purulent material prompted sampling for microbiological assessment. The lesion was drained and the remaining cavity was thoroughly irrigated with saline. Histological examination of the lesion revealed columnar epithelial cells characteristic of RCC, some of which were ciliated, resting on connective tissue. Admixed inflammatory cells were also observed including quite numerous neutrophils (Fig. 2). The histological differential diagnosis included abscess, pituitary apoplexy and RCC with superimposed inflammation. While histological examination suggested pituitary apoplexy as an alternative pathology, this was not consistent with the clinical presentation. Although initial gram stain was negative for organisms, the pus retrieved grew Staphylococcus aureus sensitive to flucloxacillin and fusidic acid on microbiological culture. The overall picture was suggestive of abscess formation within a RCC.
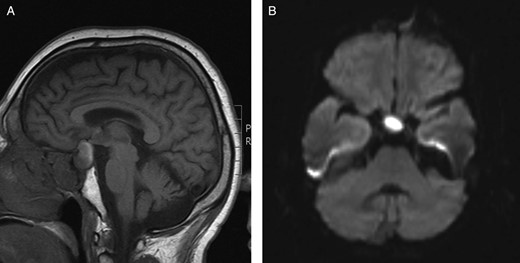
(A) Preoperative sagittal T1-weighted MRI showing a predominantly isointense lesion in the pituitary fossa with some high signal posteriorly. (B) Preoperative axial diffusion-weighted MRI demonstrating a hyperintense lesion in the pituitary fossa.
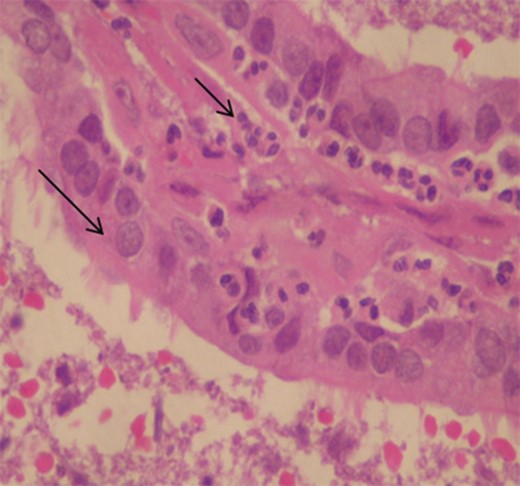
Histological image illustrating the cyst wall composed of ciliated columnar epithelium characteristic of RCC lying on a thin layer of fibrous tissue (long arrow) with infiltration by numerous neutrophils (small arrow; haemotoxylin and eosin original magnification ×400).
Postoperatively, the patient received empirical parenteral antibiotics and endocrine replacement therapy. Subjective visual function reportedly improved such that he could read a smaller font on his e-reader. Other than a short-lived delirium, the patient's postoperative course was uneventful and he was discharged home with a 3-month course of oral flucloxacillin and fusidic acid antibiotics (1 g four times daily and 500 mg twice daily, respectively) on the fifth postoperative day. Postoperative MRI scanning revealed a small residual RCC with no compression of the optic chiasm evident, which remained stable during follow-up. The patient remained clinically well at 24 months of follow-up.
DISCUSSION
Although the identification of RCCs has become more common with the advent of MRI, abscess formation within a RCC remains an unusual condition and difficult to identify preoperatively. The majority of the previously reported cases of RCC abscess have presented with clinical features typical of mass effect, namely; visual impairment, endocrine disturbance and headache [3]. Systemic features such as leukocytosis and pyrexia are atypical but may also manifest [3–5]. The majority of RCC abscesses seem to occur spontaneously, although previous pituitary surgery, irradiation of the gland and immunosuppressive therapy are speculated to be risk factors [1, 2]. Although haematogenous spread and direct extension of adjacent infection such as sphenoid sinusitis, thrombophlebitis or a contaminated cerebrospinal fluid fistula have been postulated as means by which RCCs become infected. Patients typically lack evidence of infection elsewhere [3].
Unfortunately, MRI is not specific in identifying pituitary abscess as the signal intensity of an abscess may be affected by its protein content or the presence of haemorrhage. MRI may demonstrate a pituitary abscess as a generally homogenous cystic lesion, typically hyperintense on T2-weighted images and isointense on T1-weighted images, surrounded by a ring of contrast enhancement, although this appearance is variable [6]. Some pituitary abscesses may also show high signal intensity on diffusion-weighted MRI [5]. Other sellar lesions which may exhibit a restriction of diffusion on MRI include macroadenomata, apoplexy and autoimmune hypophysitis. Although restricted diffusion was demonstrated in our case (Fig. 1B), the ambiguous clinical and radiological features focused our preoperative suspicions on commoner pathology (i.e. a macroadenoma). While autoimmune hypophysitis may present clinically and radiologically in a similar fashion, the characteristic histopathological finding of lymphocytic infiltration within pituitary tissue was absent. Although not apparent in our case, secondary pituitary abscesses may share radiological characteristics with the lesions from which they arise [6].
Diagnosis of RCC abscess is usually made with a combination of intraoperative observations and histological examination. Culture of the pus retrieved from an abscess associated with a RCC (as with most other pituitary abscesses) is typically sterile, although organisms were grown in our case together with a third of the previously reported cases [3]. Organisms isolated from RCC abscesses include both Gram-positive cocci and Gram-negative bacilli. Sterile cultures may result from an inadequate bacteriological technique or from antibiotic therapy commenced prior to or during surgery. While specimens derived via the transsphenoidal approach to the pituitary are liable to microbiological contamination, we believe that the combination of intraoperative observations and radiological, histological and microbiological findings were together highly suggestive of an RCC abscess in our case.
In common with other brain abscesses, treatment typically includes surgical drainage together with a prolonged course of antibiotics directed against an offending organism. The transsphenoidal surgical approach is preferable to avoid possible intracranial spread of infection [1]. The insertion of a pituitary-nasal drain has been employed by some for intractable cases of recurrent abscess formation [7]. A craniotomy may rarely be appropriate when the transsphenoidal approach is unlikely to provide adequate evacuation of the abscess cavity and suitable decompression of the suprasellar structures [1]. Postoperatively, careful consideration should be paid to potential concurrent sources of infection. Since endocrine dysfunction is more likely following treatment for a secondary pituitary abscess, patients may also require endocrine replacement therapy [1–3].
A close clinical and radiological follow-up is advised together with a prolonged course of antibiotics to treat any residual infection and prevent recurrence. Abscess associated with RCC has recurred in cases several months later, while RCCs may recur even many years later [8–10]. A high clinical suspicion of abscess or RCC recurrence is recommended for the rest of the patient's life; however, the risk of recurrence is likely to decrease with time.
Although rare, we recommend the consideration of RCC abscess as a differential diagnosis of a pituitary mass lesion as clinical presentation and radiological assessment are not specific in identifying these lesions preoperatively.
CONFLICT OF INTEREST STATEMENT
None declared.



