-
PDF
- Split View
-
Views
-
Cite
Cite
Ahmed Hamad, Kanagaraj Marimuthu, Bhavani Mothe, Magdi Hanafy, Repair of massive inguinal hernia with loss of abdominal domain using laparoscopic component separation technique, Journal of Surgical Case Reports, Volume 2013, Issue 3, March 2013, rjt008, https://doi.org/10.1093/jscr/rjt008
Close - Share Icon Share
Abstract
Giant inguinoscrotal hernias present a challenging surgical problem and are associated with high morbidity and mortality. The main difficulty is that of returning herniated viscera to an abdominal cavity accustomed to being empty, also known as loss of domain. In our case, we present laparoscopic component separation as a technique to increase capacity of the abdominal cavity to facilitate closure and reduce postoperative complications in those patients.
INTRODUCTION
Giant inguinoscrotal hernias are uncommon. They are defined as hernias extending below midpoint of the inner thigh in the standing position [1]. They usually present with significant implications to patients' quality of life, including difficulties with mobility, retention of urine, bowel obstruction and scrotal skin ulceration. Reduction of hernial contents may produce alterations in intraabdominal and intrathoracic pressures, precipitating cardiac or respiratory failure [2, 3]. The risk of wound dehiscence and hernia recurrence is also greater with forced closure with a recurrence rate of up to 30% [4].
Techniques described to address the loss of domain include debulking of abdominal contents by total colectomy and omentectomy [5], right hemicolectomy and small bowel resection [6]. However, this is limited by the additional morbidity and potential mortality associated with resection of abdominal viscera [2].
Other described techniques include phrenectomy, creation of a ventral hernia with repair using Marlex mesh and scrotal skin flaps and preoperative artificial pneumoperitoneum [4, 7, 8].
CASE REPORT
A 69-year-old man presented with over 10-year history of a left inguinoscrotal hernia which eventually became incarcerated with increasingly difficult urination. His quality of life had become significantly affected over the past year when he had recurrent episodes of acute urine retention that required long-term catheter. The patient also had significant issues with his mobility. He had no significant co-morbidities or surgical history. Examination revealed a massive left inguinoscrotal hernia that descended to below the level of his knees in the standing position (Fig. 1). There was no evidence of inflammation, excoriation or ulceration of the scrotal skin and no focal tenderness over the hernia.

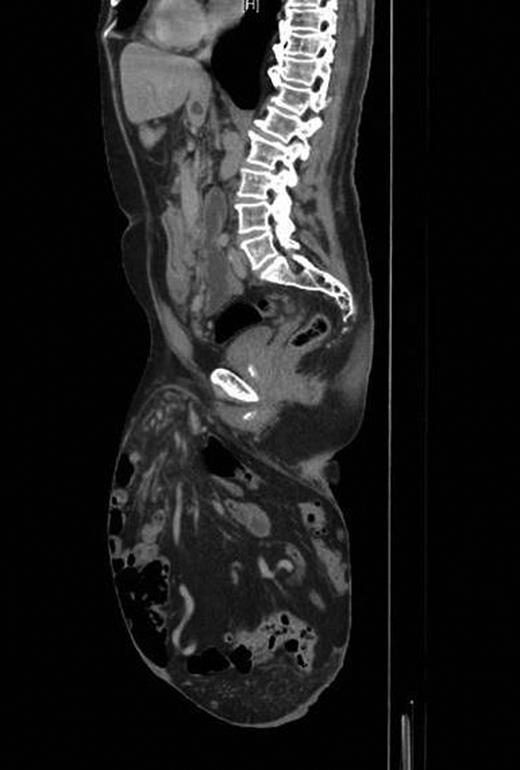
A contrast-enhanced computed tomography (CT) scan revealed the hernia sac containing most of the colon and small bowel with only the rectum, proximal jejunum and duodenum lying within the abdomen (Fig. 2). Preoperative anaesthetic assessment was completed and the patient was admitted to hospital 2 days preoperatively for bowel preparation. After a midline laparotomy, attempts at reduction were not successful even after dividing the inguinal ligament. Reduction in hernia contents was possible only after completely dividing the lower end of the left rectus abdominis muscle. The hernial sac was then dissected and resected. Then, component separation technique was performed laparoscopically using the same balloons used for total extra peritoneal (TEP repair for inguinal hernias). A 2 cm transverse incision located just under the rib cage in the mid-clavicular line was deepened until the area just posterior to the external oblique was entered. The large balloon was inserted in this space in the direction of the pelvis and inflated under laparoscopic guidance to create the space between the external and internal obliques. This was followed by the triangular balloon and insufflation was started at pressure of 11 mmHg under laparoscopic control. A lateral incision to introduce a 5 mm trocar is performed and a pair of laparoscopic scissors introduced to make a longitudinal incision in the external oblique aponeurosis extending along the mid-clavicular line from the rib cage to the inguinal ligament. The same is repeated on the other side. The hernia defect was then repaired extraperitoneally using a large polypropylene mesh extending from the anterior superior iliac spine to the symphysis pubis. Both the inguinal ligament and rectus abdominis muscle were repaired. The procedure ended by mass closure of the laparotomy incision.
Postoperatively, the patient had continuing respiratory support in high dependency unit, physiotherapy and scrotal support. Recovery was satisfactory with early return of bowel movement and mobilization. He had no significant postoperative complications and was discharged home with an indwelling urinary catheter on postoperative day 13.
On follow-up after 8 weeks, the patient was in a very good general condition with intact hernia repair and laparotomy wound. He was found to have a moderate scrotal swelling (Fig. 3) which proved by CT scan to be a postoperative seroma (Fig. 4) which was managed conservatively.


Postoperative CT scan showing intact repair and clear fluid in the scrotum.
DISCUSSION
Giant inguinoscrotal hernias present a challenging surgical problem and are associated with high morbidity and mortality associated with returning herniated viscera to an abdominal cavity accustomed to being empty, also known as loss of abdominal domain.7,9 With careful planning, patient selection and multi-disciplinary team approach, laparoscopic component separation presents a good surgical alternative to address the problem of loss of domain in those patients with less morbidity and mortality.



