-
PDF
- Split View
-
Views
-
Cite
Cite
Cara R. Baker, James A. Gossage, Robert C. Mason, An unusual cause of dysphagia: transabdominal Roux-en-Y cyst-jejunostomy in the surgical management of a symptomatic mediastinal cyst, Journal of Surgical Case Reports, Volume 2013, Issue 3, March 2013, rjs042, https://doi.org/10.1093/jscr/rjs042
Close - Share Icon Share
Abstract
We present a 52-year-old gentleman with an unusual cause of progressive dysphagia, namely due to extrinsic lower oesophageal compression from a cystic mass of the posterior mediastinum. Cystic masses in adults are uncommon, and there is a wide differential diagnosis. This includes neoplastic, such as germ cell tumour (cystic teratoma), and non-neoplastic aetiologies. The later include foregut duplication cysts, lymphatic malformations, infective (hydatid), simple mediastinal cysts or pseudocysts. Management is principally surgical with complete excision, or alternatively, in cases of benign cysts, marsupialization or decompression. In our patient, a simple mediastinal cyst was diagnosed and this case is the first description of a totally transabdominal approach to mediastinal cyst decompression by a Roux-en-Y cyst-jejunostomy.
INTRODUCTION
Cystic lesions of the mediastinum are uncommon and have a diverse aetiology and presentation. Those in the posterior mediastinum are often duplication cysts, i.e. congenital abnormalities of foregut embryonic origin. Following identification, options for management usually involve a thoracic approach to resection. Here present an unusual case of a posterior mediastinal cyst causing oesophageal displacement and dysphagia and a unique transabdominal approach to decompression with a Roux-en-Y cyst-jejunostomy.
CASE REPORT
A 52-year-old gentleman, otherwise well, presented with a 3-month history of progressive dysphagia, unable to tolerate solids. An upper gastrointestinal (GI) endoscopy showed extrinsic compression of the lower oesophagus from the posterior aspect, with normal oesophageal mucosa and no gastric abnormality. CT and MRI scanning (Fig. 1) revealed the cause of the compression to be a cystic mass (9.8 × 6.4 × 6.3 cm) in the posterior mediastinum, at the level of the inferior wall of the heart causing compression of the left atrium and displacing the oesophagus to the left (Fig. 1c). The lesion had low attenuation with dependent calcified debris.
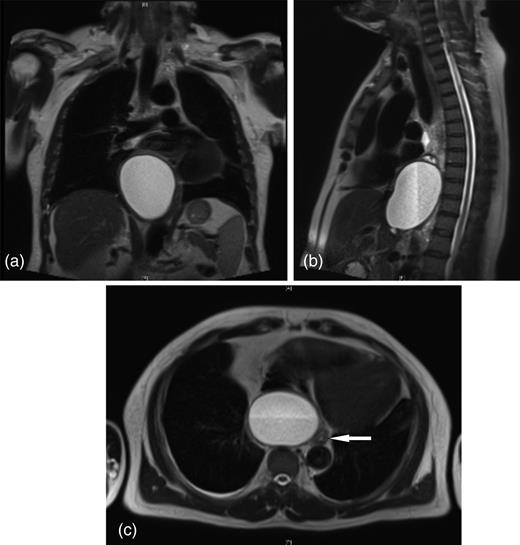
Posterior mediastinal cyst causing displacement of the distal oesophagus extending through the diaphragmatic hiatus into the retroperitoneum (a) coronal (b) sagittal and (c) transverse views (arrow denotes oesophagus).
Endoscopic ultrasound (EUS) confirmed the cyst extended to the diaphragmatic hiatus and showed no clear connection to the oesophagus or adjacent structures, concluding the lesion to be a duplication cyst. Further investigations included negative hydatid serology and a PET-CT scan with no uptake of tracer. EUS-guided fine needle aspirate of the fluid within the cyst was acellular with no microbial growth, but had a raised amylase of 1869 IU/l.
A diagnosis of a foregut duplication cyst was made and, following multidisciplinary discussion, as the patient was significantly symptomatic surgery was performed. Approaches considered included transthoracic, abdominal or combined. To avoid the potential morbidity of a transthoracic approach, an abdominal approach was performed through a rooftop incision. At surgery, a firm retroperitoneal cyst was evident emerging through the hiatus (Fig. 2a), anterior to the aorta, displacing the distal oesophagus and gastro-oesophageal junction. The cyst wall was opened and 300 ml of turbid fluid aspirated (Fig. 2b). Following wall biopsy, a jejunal loop was mobilized and a 60 cm Roux-en-Y cyst-jejunostomy performed with single-layer 2-0 PDS (Fig. 2c and d). Histology of the cyst wall revealed fibrous tissue with no obvious epithelial or mesothelial lining compatible with a simple mediastinal cyst. There was no evidence of malignancy.
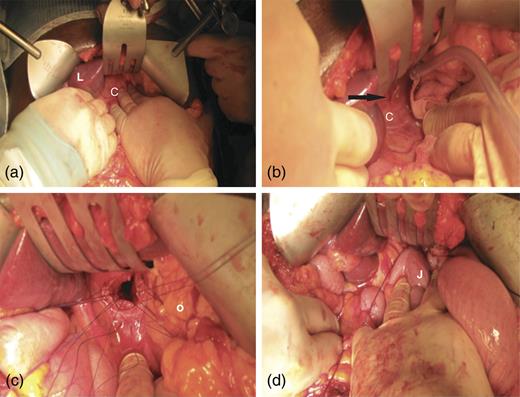
(a) Rooftop laparotomy revealing retroperitoneal cyst emerging though the diaphragmatic hiatus (C, cyst, L, liver). (b) Arrow denotes serous fluid emerging from cyst wall following needle puncture. (c) Opening of cyst below diaphragmatic hiatus with interrupted 2-0 PDS sutures to cyst wall. O, oesophagus. (d) Completed Roux-en-Y cyst-jejunostomy for mediastinal cyst drainage. J, jejunum.
Postoperatively, the patient experienced immediate relief of his dysphagia and was discharged home with no complications. He remains well and asymptomatic on follow-up.
DISCUSSION
Mediastinal cystic masses are diverse in origin and presentation. Classification can be on the basis of neoplastic and non-neoplastic lesions, the latter largely congenital in nature. A clue to origin can be found according to the mediastinal compartment in which they arise [1]. In the anterior compartment, thymic cysts, cystic teratoma, germ cell tumours and lymphatic malformations arise. In the middle compartment, pericardial cysts and foregut duplications. In the posterior compartment, lymphatic malformations, myelomeningoceles and foregut duplications (bronchogenic cyst, oesophageal duplication, neurenteric cyst).
Duplication cysts arise due to disturbances in embryonic development of the GI tract and tend to be thin walled with a smooth muscle layer and an internal mucosa arising from foregut epithelium. Alternatively, cysts of lymphatic origin characteristically are lined by flattened endothelial cells, with smooth muscle fibres and lymphoid tissue within the wall [2].
Presentation with symptoms is more common in the paediatric population where compressive symptoms can predominate. In adults, mediastinal cysts are often an incidental finding on imaging. If symptomatic, they do so by compression of local structures or if contain ectopic gastric or pancreatic mucosa, can ulcerate, bleed or perforate precipitating an acute presentation.
Pathological diagnosis is often required to confirm the exact nature of the lesion. The aetiology of our patient is most likely a simple mesothelial cyst or pseudocyst, as it lacked a defined smooth muscle layer or obvious bronchogenic, oesophageal or pancreatic epithelium. Our patient had no history or imaging findings that could have related to an episode of pancreatitis, nor an obvious traumatic or infective precipitant to the aetiology.
The investigation of mediastinal cystic lesions can include imaging by CT, MRI and EUS. Management is principally surgical with complete excision, or alternatively, in cases of benign cysts, marsupialization or decompression. In our patient, with the benign findings on preoperative investigations in conjunction with raised amylase in the cyst fluid and an intimate relation to the oesophagus and left atrium, we felt the least morbid procedure was cyst decompression from an abdominal approach. Malignant change in a duplication cyst is extremely rare and surgery should address the related complications and prevent recurrence [3]. We have found only one other report in the literature of a mediastinal pancreatitis-related pseudocyst managed by a transdiaphragmatic Roux-en-Y cyst-jejunostomy; however, this case was performed by a thoracoabdominal approach [4].
In summary, we have presented an unusual case of dysphagia caused by a posterior mediastinal cyst distorting the oesophagus and a novel safe surgical approach to cyst decompression by a transabdominal Roux-en-Y cyst jejunostomy.
Conflict of interest statement. None declared.



