-
PDF
- Split View
-
Views
-
Cite
Cite
Özcan Binatli, Onur Yaman, Nail Özdemir, Işın Gökçöl Erdoğan, Pleomorphic adenoma of lacrimal gland, Journal of Surgical Case Reports, Volume 2013, Issue 10, October 2013, rjt089, https://doi.org/10.1093/jscr/rjt089
Close - Share Icon Share
Abstract
We present a case of a 62-year-old male patient with pleomorphic adenoma and painless solid mass in his right eye. Computerized tomography demonstrated a mass with a diameter of 2.5 cm located in the right lacrimal gland. The mass was removed completely by combined orbitofrontal craniotomy through a transcranial approach. Histopathologic examination revealed pleomorphic adenoma of the lacrimal gland. Orbital tumors originate primarily from vascular, muscle, cartilage, neural tissues, lacrimal glands and lymphoid structures. Five percent of all intraorbital masses originate from the lacrimal gland. Pleomorphic adenoma presents as a painless and slowly growing mass and also as exophthalmoses. Pleomorphic adenoma has a high morbidity. Morbidity increases due to the total displacement of the tumor without its capsule and incisional biopsy for the purpose of diagnosis. The success of the treatment depends on the removal of the tumor with its capsule.
INTRODUCTION
Pleomorphic adenoma of the lacrimal gland is very rare. It presents as a painless and slowly growing mass and also as exophthalmoses like in orbital masses. Pleomorphic adenoma has a high morbidity. This study aims to identify the clinical course, surgical treatment and histopathologic properties of pleomorphic adenoma diagnosed in a patient who had painless exophthalmia with an intraorbital mass.
CASE REPORT
A 62-year-old male patient referred to our clinic due to painless exophthalmia of his right eye for the last 2 years. On neurological examination of the patient, there was no abnormality except for the up-gaze restriction and severe exophthalmia. Computerized tomography revealed an intraorbital mass in the right eye. A well-defined 2.5-cm isodense mass was located on the right lacrimal gland. The mass was contrasted homogenously (Fig. 1a and b). Cranial magnetic resonance imaging (MRI) revealed an isointense mass on the superolateral part of right orbita in the coronal intersections and it was contrasted homogenously (Fig. 2a and b). The existing score of our patient according to Rose and Wright was +8 points. Combined orbitofrontal craniotomy was performed through a transcranial approach. The well-defined, soft, white, 2.5-cm mass was removed completely. Exophthalmoses disappeared after the surgery (Fig. 3a and b). Histological examination of the surgical specimen covered the epithelial and stromal components that formed the glandular structures. Keratinized plugs were seen in some glandular lumens. Cartilaginous differentiation of stroma was found (Fig. 4a–d). Based on these findings, the tumor was diagnosed as pleomorphic adenoma. There was no recurrence after 8-year clinical follow-up.
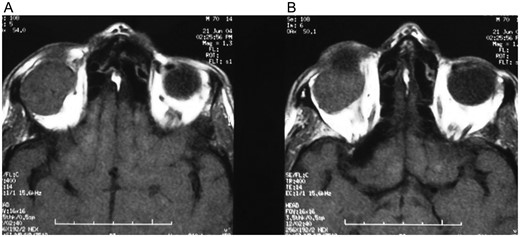
(A and B) Computerized tomography revealed a homogenously contrasted intraorbital mass in the right eye.
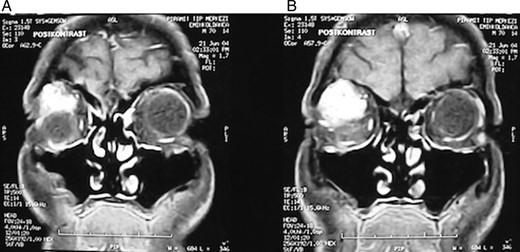
(A and B) Cranial MRI revealed a homogenously contrasted mass on the superolateral part of the right orbita.
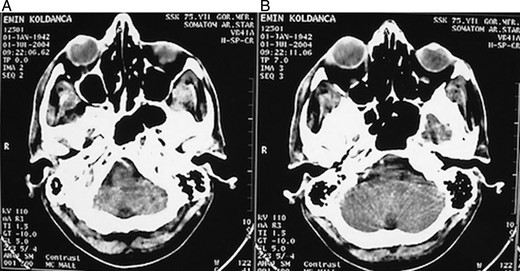
(A and B) Postoperative computerized tomography revealed the replacement of the eye.
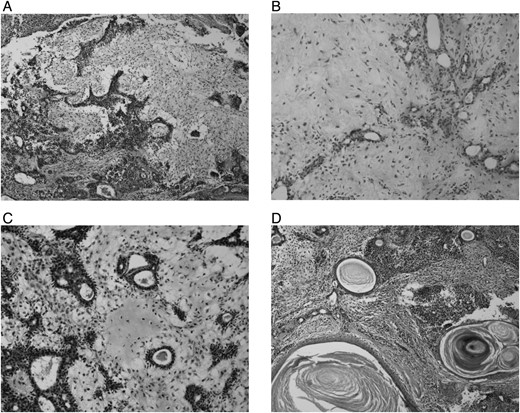
(A) Four times H-E biphasic tumor composed of epithelial and stromal components. (B) Ten times H-E fibromyxoid stroma and epithelium that form glandular structures. (C) Twenty times H-E cartilaginous focus in the stroma. (D) Four times H-E keratinized plugs in some glandular lumens.
DISCUSSION
Although the orbital tumors originate primarily from vascular, muscle, cartilage, neural tissues, lacrimal glands and lymphoid structures, they can also originate from the surrounding structures and (low possibility of) metastasis. Five percent of all intraorbital masses originate from the lacrimal gland. The majority of the lacrimal fossa lesions consist of inflammatory lesions. Epithelial tumors account for 30% of the lacrimal gland lesions, while 12% of epithelial tumors are pleomorphic adenoma [1]. Ferry et al. [2] reported a case with a secondary metastasis to the lacrimal gland. Bilroth described the fact that pleomorphic adenoma consisted of epithelial and mesenchymal components [3]. The term pleomorphic (benign mixed tumor) was first defined and used by Willis. Adenoid cystic carcinoma and adenocarcinoma are the other epithelial tumors of the lacrimal gland [4]. Malignant transformation can occur in 10–20% of pleomorphic adenomas of the lacrimal gland [5, 6]. Seventy-five percent of pleomorphic adenomas transform into pleomorphic adenocarcinoma, while the rest transform into cystic carcinoma [6].
A limited number of cases with lacrimal pleomorphic adenoma were reported [7]. Pleomorphic adenoma presents as a painless and slowly growing mass and also as exophthalmoses. Pleomorphic adenoma must be considered for the patients whose clinical course lasts for 12 months [8]. Malignancy must be considered for cases with pain and progredien symptoms. In his study, Wright reported that 39 of 40 cases diagnosed with primary malignant lacrimal gland tumors had a painful mass [6]. In addition to pain, neoplasm of the lacrimal gland, which destroys the bones, can be interpreted as malignancy. While pleomorphic adenomas do not destroy the bones, malignant neoplasm does [9, 10]. The histology of the lacrimal gland lesion cannot be determined via MR images [9].
Although pleomorphic adenomas constitute 4–9% of all orbital tumors, their morbidity is very high [3]. Displacement of the mass without its capsule and malignant transformations following the incisional biopsies prior to the diagnosis of pleomorphic adenoma increase the morbidity. To this end, Rose and Wright developed a scoring system to evaluate the lacrimal gland masses [6, 9] (Table 1). According to this scoring system, if the value obtained from this table is below +2, the value may indicate carcinoma and thus incisional biopsy can be performed. The values +3 and higher may indicate pleomorphic adenoma and thus, incisional biopsy must not be performed. Excisional biopsy can be performed, if needed. The success of the treatment depends on the displacement of the mass with its capsule. Any defect on the capsule causes the myxoid part to effuse and relapse. It can also lead to malignant transformation of pleomorphic adenoma. The existing score of our patient according to Rose and Wright was +8 points. It looked like a typical pleomorphic adenoma. Combined orbitofrontal craniotomy was performed without any incisional biopsy. The mass and its capsule were completely removed. There was no relapse observed during 8-year follow-up of the patient.
| Clinical . | SCORE . | . |
|---|---|---|
| −1 | +1 | |
| Duration of acute symptoms | <10 months | >10 months |
| Persistent pain | Present | Absent |
| Sensory loss | Present | Absent |
| Radiological | −1 | +1 |
| Well-defined round or oval mass | Absent | Present |
| Moulding of mass to globe or along the lateral orbital wall | Present | Absent |
| Tumor calcification | Present | Absent |
| Invasion of bone | Present | Absent |
| Duration of symptoms in relation to tumor size | Short symptoms | Long symptoms |
| Clinical . | SCORE . | . |
|---|---|---|
| −1 | +1 | |
| Duration of acute symptoms | <10 months | >10 months |
| Persistent pain | Present | Absent |
| Sensory loss | Present | Absent |
| Radiological | −1 | +1 |
| Well-defined round or oval mass | Absent | Present |
| Moulding of mass to globe or along the lateral orbital wall | Present | Absent |
| Tumor calcification | Present | Absent |
| Invasion of bone | Present | Absent |
| Duration of symptoms in relation to tumor size | Short symptoms | Long symptoms |
| Clinical . | SCORE . | . |
|---|---|---|
| −1 | +1 | |
| Duration of acute symptoms | <10 months | >10 months |
| Persistent pain | Present | Absent |
| Sensory loss | Present | Absent |
| Radiological | −1 | +1 |
| Well-defined round or oval mass | Absent | Present |
| Moulding of mass to globe or along the lateral orbital wall | Present | Absent |
| Tumor calcification | Present | Absent |
| Invasion of bone | Present | Absent |
| Duration of symptoms in relation to tumor size | Short symptoms | Long symptoms |
| Clinical . | SCORE . | . |
|---|---|---|
| −1 | +1 | |
| Duration of acute symptoms | <10 months | >10 months |
| Persistent pain | Present | Absent |
| Sensory loss | Present | Absent |
| Radiological | −1 | +1 |
| Well-defined round or oval mass | Absent | Present |
| Moulding of mass to globe or along the lateral orbital wall | Present | Absent |
| Tumor calcification | Present | Absent |
| Invasion of bone | Present | Absent |
| Duration of symptoms in relation to tumor size | Short symptoms | Long symptoms |
Pleomorphic adenoma of the lacrimal gland must be considered in the presence of long-term painless exophthalmoses. For the patients suspected to have pleomorphic adenoma, incisional biopsy should not be performed in order to prevent the likelihood of a relapse to occur. The displacement of the mass with its capsule can extend the patients' lives and improve their quality of life.



