-
PDF
- Split View
-
Views
-
Cite
Cite
Nathan C. Tiedeken, Vilas Saldanha, John Handal, James Raphael, The irreducible floating hip: a unique presentation of a rare injury, Journal of Surgical Case Reports, Volume 2013, Issue 10, October 2013, rjt075, https://doi.org/10.1093/jscr/rjt075
Close - Share Icon Share
Abstract
A floating hip injury occurs in the setting of poly-trauma and is a rare and difficult problem to manage. Floating hip injuries require vigilant attention not only to the osseous injuries but also the surrounding compartments and soft tissue envelope. We report the case of a 35-year-old male with a lower extremity posterior wall acetabular fracture, ipsilateral femoral shaft fracture and a postero-superior hip dislocation. Closed reduction failed, necessitating an open reduction internal fixation of his hip dislocation and acetabular fracture. The patient then developed a thigh compartment syndrome requiring a fasciotomy. Despite the obvious bony injuries, orthopedic surgeons must be vigilant of the neurovascular structures and soft tissues that have absorbed a great amount of force. A treatment plan should be formulated based on the status of the overlying soft tissue, fracture pattern and the patient's physiologic stability.
INTRODUCTION
A ‘floating hip’ is defined as a fracture of the pelvis or acetabulum with a concomitant femur fracture [1, 2]. This combination of injuries is uncommon and estimated to occur once in every 10 000 fractures [3, 4]. Anterior and posterior dislocations of the ipsilateral hip can be associated with this injury [1, 4–6]. This fracture/dislocation pattern occurs commonly in young males involved in high-energy automotive/motorcycle trauma [1, 6–10]. Under these circumstances, damage control orthopedics should be applied as other life-threatening injuries are addressed [2, 8]. Floating hips can be divided into two categories. Type A includes a fracture of the pelvic ring and femur, whereas type B includes a fracture of the acetabulum and femur. Regardless of the mechanism of injury, the surrounding soft tissues of the affected extremity encounter an incredible amount of force. Sciatic nerve palsy occurs in 26–35% of floating hip injuries, an incidence greater than with acetabular fractures alone [2, 3, 7, 8]. Floating hips with associated vascular injuries have a very poor outcome and frequently results in an above-knee amputation despite immediate vascular repair [5].
We present the case of a 35-year-old male with an irreducible floating hip with the development of thigh compartment syndrome. Previous cases of irreducible anterior floating hips have been reported, but we describe the first case of a posterior irreducible floating hip injury [6]. Injuries associated with floating hips are well reported in the literature, but no documentation of compartment syndrome has been described. The bony fixation of a floating hip injury has garnered much attention since its first description in the 19th century, but the importance of assessing the soft tissues must not be overlooked.
CASE REPORT
A 35-year-old male was involved in a high-speed urban dirt biking accident. The patient was stable with a GCS of 15 and was neurovascularly intact. His left knee exhibited a 10 × 20 cm medial traumatic arthrotomy and his thigh compartments were soft and compressible. Imaging revealed a left hip postero-superior dislocation, posterior wall acetabular fracture, ipsilateral transverse femoral diaphyseal fracture and an engaging hill-sachs-type lesion of the femoral head with the postero-superior acetabulum (Figs 1–3). Cefazolin, gentamicin and tetanus prophylaxis were administered along with a bedside washout of the traumatic arthrotomy. The patient was medically cleared for operative intervention as all blood work and further imaging were normal.

AP left hip demonstrating a diaphyseal transverse femur fracture with ipsilateral hip dislocation.

AP left femur of type B floating hip with associated hip dislocation. The medial knee soft tissue injury is also appreciated.
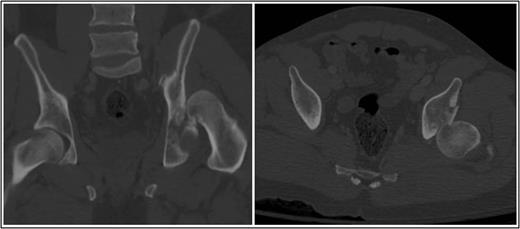
Coronal and axial CT pelvis of the left femoral head engaging with the postero-superior acetabulum.
Operative management focused on closed reduction of the dislocated left hip. Two 5.0 mm Schanz pins with a carbon fiber bar (Zimmer, Warsaw, Indiana, USA) were placed in the proximal femur fragment. This was used to aid with the closed reduction maneuver of knee flexion, hip traction, adduction and internal rotation. Confirmed by intra-operative fluoroscopy, the femoral head was irreducible due to the engaging femoral head lesion on the acetabulum. A conversion to open reduction via a Kocher–Langenbeck approach in the lateral position ensued. The femoral head and posterior wall were reduced under direct visualization with two 3.5 mm pelvic reconstruction plates (Zimmer). The patient was moved to the supine position and underwent definitive femoral fixation with a retrograde, reamed femoral nail (Zimmer). Thigh compartments at the conclusion of the femoral fixation were tense and non-compressible, requiring a thigh compartment fasciotomy. Negative pressure therapy was placed over the incision and the knee laceration was primarily closed. After multiple washouts of his lateral fasciotomy incision, he was primarily closed 1 week after initial presentation. He was discharged non-weight bearing on his left lower extremity on post-operative day 22. Eleven months post-injury, he remains full weight bearing without assistance. He reports intermittent pain with ambulation and radiographs show early arthritic changes and heterotopic ossification of his left hip (Fig. 4).

AP pelvis 8 months status post-ORIF of posterior wall with retrograde femoral nail. The left hip demonstrates early post traumatic arthritis and heterotopic ossification.
DISCUSSION
In the face of high-velocity trauma, the clinician must remain vigilant for the development of compartment syndrome. Our patient initially presented with soft compartments that evolved into a clinical diagnosis of compartment syndrome after femoral length was restored. To the authors' knowledge, this is the first reported case of an irreducible posterior floating hip injury. Despite previous attempts to standardize a sequence of fixation for floating hips, the complexity of this injury emphasizes that each case must be managed on an individual basis.
The floating hip is the result of high-energy trauma and presents many challenges to the trauma team. While femur fractures are readily observed on routine X-ray, >50% of hip dislocations can be missed with floating hip injuries [6]. The femur fracture behaves as a corrective osteotomy masking the typical rotational deformities of an uncomplicated hip dislocation [6]. This underscores the importance of radiographic examination of both the joint above and below a fracture in the poly-trauma population. Although reduction of a floating hip dislocation is difficult, multiple closed techniques utilizing Steinmann pins and traction bows have been described with excellent success [1, 4, 5, 10]. We present the first case of an irreducible type B posterior floating hip and its subsequent management.
Much debate has been devoted to the proper management of this combination of skeletal injuries [10]. Attempts to form a protocol for the timing and sequence of pelvis and femoral fixation has yielded to a ‘damage control’ approach emphasizing the patient's physiologic status and associated injuries [1, 4, 7, 8, 10]. External fixation provides a method of temporary stability for both pelvic and long bone fractures and has been utilized frequently in the initial treatment for floating hips. A majority of the literature regarding floating hip injuries focuses on femoral fixation preceding definitive management of pelvic and acetabular fractures [7, 10]. Unfortunately, many of these reports did not exhibit an associated hip dislocation. Our patient presented with a hip dislocation which mandated emergent reduction within 6 h of the injury to reduce the risk of avascular necrosis to the femoral head. The Kocher–Langenbeck approach provided excellent visualization of the posterior acetabular fracture and reduction of the femoral head. Early fixation and reduction of acetabular fractures permits mobilization and correlates with improved clinical outcomes. The physiologic stability of our patient permitted operative hip reduction within 4 h of injury and definitive fixation of all fractures. Implementing the principles of damage control orthopedics, assessing the soft tissue condition, and understanding the injury pattern are critical in achieving an optimal outcome for floating hip injuries.



