-
PDF
- Split View
-
Views
-
Cite
Cite
H Chim, HT Soltanian, Spontaneous compartment syndrome of the forearm in association with nephrotic syndrome and transient bacteremia, Journal of Surgical Case Reports, Volume 2012, Issue 8, August 2012, Page 11, https://doi.org/10.1093/jscr/2012.8.11
Close - Share Icon Share
Abstract
We present a patient with spontaneous compartment syndrome of the upper extremity in association with nephrotic syndrome and transient bacteremia, of which the exact cause of compartment syndrome was unclear. This is an extremely rare occurrence, and index of suspicion should be maintained even in the absence of trauma when a patient presents with acute swelling of the upper or lower extremity together with nephrotic syndrome.
INTRODUCTION
Compartment syndrome is a surgical emergency involving the upper extremity and occurs when elevated interstitial pressure in a confined osteofascial compartment results in microvascular compromise. Common causes are well known and include trauma, burns and vascular injury. However, rarer spontaneous causes are less often encountered, and include association with diabetes mellitus, leukemic infiltration, anticoagulation, and hypothyroidism (1). We report a case of spontaneous compartment syndrome in association with nephrotic syndrome.
CASE REPORT
A 15-year-old male with nephrotic syndrome diagnosed at 1 year of age presented with acute onset of right forearm swelling and pain over 2 days, worsening acutely over 8 hours prior to consultation by the plastic surgery service. He denied any precipitating trauma or inciting event. On examination he was found to have tense swelling over the proximal dorsal aspect of his forearm, with severe pain on passive flexion of his wrist and fingers. Radial and ulnar pulses were palpable, and sensation was intact to all fingers. Compartment pressures were measured, and showed elevated pressures in the dorsal forearm compartment of 70 mmHg, with a volar forearm compartment pressure of 14 mmHg. MRI had previously been ordered by the pediatric medicine service, and showed muscle edema concerning for myositis in the dorsal compartment of the forearm (Fig. 1). Due to swelling localized to the dorsal forearm as well as elevated pressures in the dorsal forearm compartment only, the presumptive diagnosis was compartment syndrome localized to the dorsal forearm compartment.
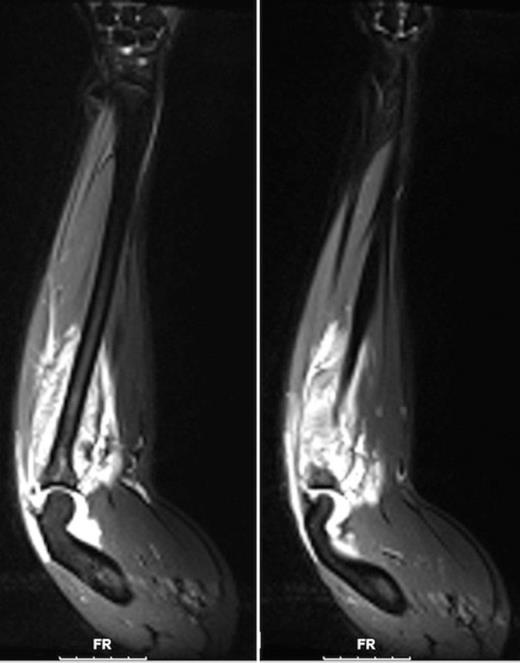
MRI of the forearm (coronal sections) shows enhancement on T2-weighted images suggesting edema in the region of the ulna (left) and dorsal forearm musculature (right).
The patient also concurrently had a small chin abscess measuring around 1 cm in diameter, which required incision and drainage prior to the onset of the right forearm swelling. Culture from the chin abscess grew methicillin sensitive Staphylococcus Aureus (MSSA). Hence he was treated with intravenous Cephazolin, continued during the perioperative period. However, blood cultures on multiple occasions were negative. Hematological investigations showed a leukocytosis of 19.6 x 109/L, while creatinine kinase was normal at 34 U/L.
He was brought emergently to the operating room where decompression of the dorsal compartment of the forearm was carried out. All muscles were found to be healthy and viable, with no gross evidence of infection. There was no evidence of pus or fluid in the compartment and only minimal swelling of the muscles. Cultures from the forearm were negative. After decompression of the dorsal compartment, the volar compartment and mobile wad appeared soft. In view of the normal volar compartment pressure measured prior to surgery as well as MRI evidence of swelling only confined to the dorsal compartment, we decided not to decompress the volar compartment and mobile wad, and avoid the morbidity of a separate incision. Following fasciotomy, his clinical symptoms and leukocytosis resolved.
DISCUSSION
Spontaneous compartment syndrome in association with nephrotic syndrome is a very rare occurrence, with only one other case report occurring in the lower extremity (2). The pathogenesis of edema in nephrotic syndrome is a matter of controversy, with interstitial inflammation of the kidney proposed to have a key role through inducing primary sodium retention (3). A reduction in transcapillary osmotic pressure between different upper extremities has been reported to result in edema in one extremity only in patients with nephrotic syndrome (4). The mechanism postulated for asymmetrical edema in the affected extremity was the inability to increase lymphatic flow during periods of hypoalbuminemia to levels sufficient to reduce the interstitial oncotic pressure gradient. Why a reduction in transcapillary osmotic pressure should occur only in one extremity but not the other is unclear, but lowered tissue-fluid osmotic pressure has been thought to be important for preservation of blood volume in dry patients with nephrotic syndrome (5).
The etiology of compartment syndrome in this patient is puzzling. While primary pyomyositis has been reported in children, in some cases leading to compartment syndrome (6,7), the vast majority of reported cases of pyomyositis could be treated conservatively with intravenous antibiotics. Those cases resulting in compartment syndrome were associated with gross infection and often formation of abscesses. Recently, the aggressive infection caused by localized methicillin resistant staphylococcus aureus (MRSA) has also been associated with pyomyositis and compartment syndrome (8). In the absence of gross infection or an aggressive bacterium such as MRSA, it is unusual that spontaneous compartment syndrome should occur. However, the presence of edema is a known risk factor for infection, and has been associated with cellulites and erysipelas in the extremity (9).
We postulate in this case that the patient’s pre-existing nephrotic syndrome resulted in localized edema in the right forearm. The presence of edema resulted in an infective diathesis, resulting in seeding of the muscles of the dorsal forearm by MSSA during the transient bacteremia occurring during incision and drainage of the chin abscess. As the patient was on intravenous antibiotics prior to and during surgery, this may have reduced the impact of a significant bacteremia on the forearm muscles. This resulted in myositis of the dorsal compartment of the forearm only and not elsewhere, leading to compartment syndrome requiring fasciotomy. However, it is still unclear why the muscles of one forearm should have been seeded by MSSA instead of the other forearm.
In this patient, an unusual sequence of events allowed for the development of compartment syndrome. While extremely rare, swelling and pain in the extremities in patients with nephrotic syndrome should raise the possibility of compartment syndrome with the attendant need for urgent surgical intervention.



