-
PDF
- Split View
-
Views
-
Cite
Cite
LJ Kopplin, JA Kim, Retroperitoneal sarcoma: a rare cause of intestinal perforation in two cases, Journal of Surgical Case Reports, Volume 2011, Issue 5, May 2011, Page 3, https://doi.org/10.1093/jscr/2011.5.3
Close - Share Icon Share
Abstract
Retroperitoneal sarcoma is a rare malignancy often insidious in onset. At initial presentation, abdominal mass, pain or obstructive symptoms are the most common complaints. Here we present two patients who presented with abdominal discomfort and were discovered to have retroperitoneal sarcomas with secondary intestinal perforation. Perforation is a rare complication of retroperitoneal sarcoma, but one with the potential to significantly affect patient outcomes. Both patients underwent surgical resection and pathological characterization of their malignancies. The discovery of intestinal perforation during workup necessitates initiation of empirical antibiotic coverage and prompt surgical intervention.
INTRODUCTION
Retroperitoneal sarcomas are uncommon malignancies with indolent presentations. Population estimates place the yearly incidence at 2.7 cases per million people (1). The typical presenting symptom is an abdominal mass, pain, or symptoms related to compression of adjacent abdominal structures (2-8). Review of the literature reveals that the most common ages of presentation are in the 5th or 6th decade, with similar distribution among the sexes (1,2,5-9). Presentation is often complicated by metastasis or involvement of local structures (4). Here, we report two patients who presented with retroperitoneal sarcomas that were found to be complicated by gastrointestinal perforation.
CASE REPORT
Patient A is a 67 year old female with a history of pelvic leiomyosarcoma and total abdominal hysterectomy with bilateral salpingo-oopherectomy who presented with abdominal discomfort, early satiety and weight loss. On physical exam she was noted to have a large, firm abdominal mass. Admission labs revealed a marked leukocytosis (WBC=45 700) and blood cultures positive for E. coli. CT of the abdomen and pelvis revealed a mass occupying the pelvis and majority of the abdomen with air pockets, questionable portal venous gas and mild left hydronephrosis (Figure 1).

Abdominal and pelvic CT of patient A demonstrating a large mass with air pockets (arrow).
The patient was treated with antibiotic therapy and underwent surgical resection of a 40 cm retroperitoneal and pelvic sarcoma. During the operation the right colon was noted to have perforated into the tumor, with succus entericus grossly visible. Surgical approach was broadened to include a right hemicolectomy, sigmoidectomy with colostomy and segmental small bowel resection. Pathological analysis revealed a malignant spindle cell tumor with negative immunohistochemical staining for CD117 and CD10 and mild reactivity for desmin and muscle specific actin, making low grade leiomyosarcoma the most likely diagnosis.
At three month follow-up, patient A continued her recovery and remained free of detectable cancer. Given the low grade pathology of the patient’s tumor, additional treatment with chemotherapy or radiation was considered unnecessary.
Patient B is a 61 year old male who presented with abdominal pain and weight loss. Physical exam revealed a palpable mass in the left lower quadrant. At presentation he demonstrated a leukocytosis (WBC=76 800), although he was initially afebrile and demonstrated no signs of infection. Abdominal and pelvic CT showed a mass beginning at the left kidney and attached to the sigmoid colon. A CT guided biopsy demonstrated a pleomorphic high grade sarcoma consistent with malignant fibrous histiocytoma. Further evaluation with MRI demonstrated a large, necrotic mass in the left retroperitoneum that encased the descending colon with an air-fluid level concerning for a contained colonic perforation (Figure 2). The patient was started on antibiotics and taken for surgical resection.
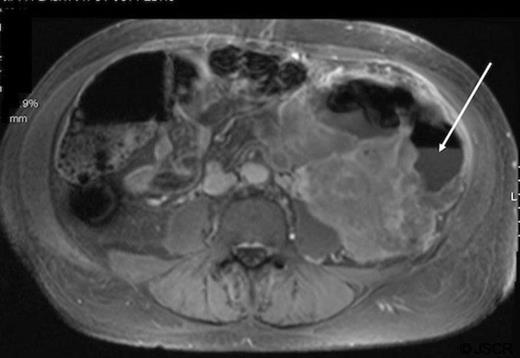
Abdominal MRI of patient B demonstrating an air-fluid level (arrow) of the descending colon with surrounding mass.
Intraoperatively, free intraperitoneal air and a small amount of fecal contamination of the retroperitoneum were noted. An en bloc resection of the left colon, retroperitoneal sarcoma, left kidney and adrenal gland with end colostomy were completed. Pathologic evaluation demonstrated strong expression of vimentin without evidence of staining for cytokeratin CAM5.2, CD15, CD30, CD117, desmin, and S100 protein, confirming the findings of pleiomorphic high grade undifferentiated sarcoma observed on biopsy.
Within three months of resection, patient B experienced recurrence of his malignancy and died.
DISCUSSION
Intestinal perforation represents a rare presenting complication of retroperitoneal sarcoma. Review of the literature (2-9) did not uncover any reports of intestinal perforation secondary to retroperitoneal sarcoma. Many of the available case series were completed prior to the widespread use of CT and MRI in evaluating abdominal complaints. This factor potentially limited the ability to identify intestinal perforations and accounts for the lack of previous descriptions. Still, review of those series reporting surgical outcomes and complications does not reveal mention of intestinal perforations as an intraoperative finding, highlighting the relative uniqueness of this occurrence.
Given patient A’s prior history of leiomyosarcoma and findings of low grade leiomyosarcoma on pathology in her current presentation, we believe this most likely represents a recurrence of her prior malignancy. Results from a large case series of retroperitoneal sarcomas found leiomyosarcomas to be the second most common form of retroperitoneal sarcoma, after liposarcomas (2). This recurrence most likely represents a slow growing malignancy that was not brought to clinical attention until quite late in the clinical course. As such, long-standing compression of the gastrointestinal tract by the malignancy probably resulted in perforation of the colon. Given the lack of prior medical history, patient B’s sarcoma seems likely to be a primary malignancy. Malignant fibrous histiocytomas are a rare subtype of sarcoma in comparison to leiomyosarcoma (2). The more aggressive nature of this sarcoma makes perforation seem likely to be secondary to rapid local growth.
Of note, at presentation both patients demonstrated significant leukocytosis. The findings of positive blood cultures in patient A indicate an infectious etiology, most likely secondary to her intestinal perforation, may underlie her leukocytosis. Patient B was found to have negative blood cultures at the time of presentation and his elevated WBC count more likely represents a leukemoid reaction.
Surgical resection remains the mainstay of treatment for retroperitoneal sarcoma (1) with resection rates ranging from 54-88% in several case series (10). Despite these efforts, local recurrence is common. Prognosis is largely related to the attainment of clear surgical margins and to the degree of differentiation of the sarcoma at the time of presentation (2). The rapid recurrence of malignancy and poorer outcome in patient B is likely a reflection of the high grade, undifferentiated nature of his sarcoma. Patient A remains free of detectable disease. She will continue to be monitored for evidence of recurrence with CT and follow up examinations every 6 months.
Gastrointestinal perforation is a rare, but clinically significant, potential complication of retroperitoneal sarcoma. Identification of such a finding during clinical workup should result in prompt initiation of antibiotics and surgical intervention.



