-
PDF
- Split View
-
Views
-
Cite
Cite
N Scott, M Patel, C Newlands, Desmoplastic fibroma of the mandible: an unusual presentation and treatment, Journal of Surgical Case Reports, Volume 2011, Issue 11, November 2011, Page 5, https://doi.org/10.1093/jscr/2011.11.5
Close - Share Icon Share
Abstract
Desmoplastic fibromas are rare, benign bone tumours, which often behave in a locally aggressive manner. In the head and neck region they are most commonly seen in the mandible and have been treated in various ways. We present an unusual presentation of the lesion, which was subsequently treated by the less commonly used technique of enucleation, with good results.
INTRODUCTION
Desomplastic fibroma of the mandible is a rare, benign but locally aggressive bone tumour that was first reported in the mandible by Griffith and Irby in 1965(1). There have been few cases reported in the literature with varying methods of treatment(2). We present one such case that presented in a different manner and treated by a less commonly reported method.
CASE REPORT
In April 2002 a general dental practitioner referred a 10-year old girl with mandibular asymmetry associated with a 6mm midline shift to the right and a Class 3 skeletal and incisor relationship. Radiographs at initial presentation showed no bony abnormalities and study models were taken, followed by a period of growth monitoring.

During the next 4 years regular review revealed no change in facial asymmetry. An 18 month course of pre-surgical orthodontic treatment was undertaken, followed by a complication free bimaxillary osteotomy in December 2006. 7 days post-operatively the patient presented with pus in the left buccal space. Subsequent examination under general anaesthesia revealed a healing osteotomy site with minimal pus and 2 loose sequestrae. The area was thoroughly irrigated and the sequestrae removed and sent for histological study in view of the fact that the operation site was otherwise healing well. The patient made an uneventful recovery and the histopathology revealed normal bone.
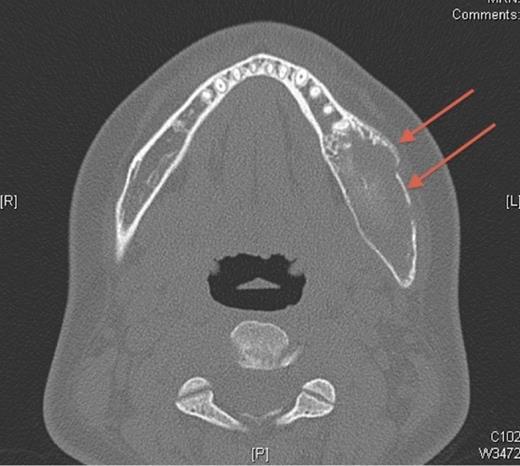
In October 2007, the patient represented with a swelling around the left angle of the mandible. Radiographs revealed no abnormalities but oral antibiotics were commenced with the clinical impression being that of osteomyelitis. Over the following month the swelling fluctuated in size, therefore a CT scan was undertaken. This showed a cystic enlargement at the left angle of the mandible with no cortical disruption or soft tissue involvement. With symptoms persisting the patient underwent exploration of the area under general anaesthesia and histopathology (which had previously been negative) now revealed desmoplastic fibroma.
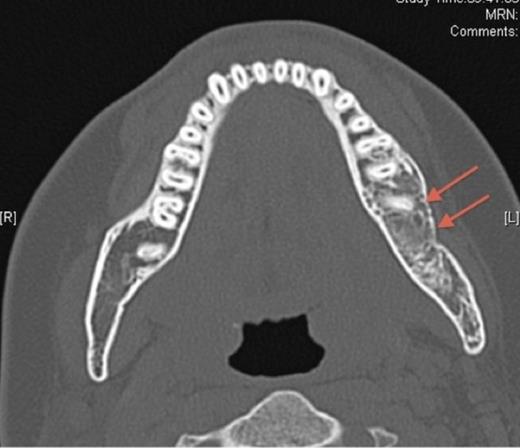
Pre-operative axial CT showing the lesion in the left side of the mandible (denoted by arrows).
Enucleation of the cystic area under general anaesthesia was undertaken, with preservation of the inferior dental bundle and the swelling completely resolved. The patient remained asymptomatic for 3.5 years when she presented with a left sided facial swelling. Subsequent examination under anaesthesia and biopsy showed no recurrence of the lesion. The swelling resolved following the removal of the bi-cortical screws placed at the initial osteotomy. Repeat CT scans have shown good bone infill of the enucleation site with no evidence of recurrence, intact ID nerve function and no further symptoms. The patient remains under review.
DISCUSSION
The WHO defines a desmoplastic fibroma as a rare, benign bone tumour composed of spindle cells with minimal atypia and abundant collagen production(3). They account for approximately 0.1% of all primary bone tumours in the body and are most commonly seen in the mandibles of adolescents and young adults(3).
A desmoplastic fibroma often behaves in an aggressive manner and macroscopically has a firm consistency with well-defined advancing surfaces that may extend into surrounding soft tissue. It is usually seen radiographically as a well-demarcated, radiolucent lesion. However, CT and MRI offer the best imaging of the lesion(5). The initial facial asymmetry in this case was most likely caused by the desmoplastic fibroma that was not evident on plain radiographic imaging. Further to this the lesion was not clinically active in the 4 years pre-operatively or evident at osteotomy. It was only in the post-operative period that the lesion was diagnosed, albeit following an initial negative histology
Although enucleation was undertaken in this case, the literature reports the most common treatment for desmoplastic fibroma being a block resection or wide local excision, with enucleation rarely used(2). The infrequent use of enucleation is due to the concern that recurrences rates are higher, approximately 20-40% compared to a minimal recurrence rate in block resection or wide local excision (2,4). A 3 year follow up period is recommended(5) and in this case we have shown no recurrence in this time with a far less traumatic procedure, shorter recovery time and less morbidity to the patient.
This lesion appears to have been less aggressive than others reported and this may have accounted for its suitability to enucleation. Therefore we would recommend a similar technique to others faced with a desmoplastic fibroma behaving in such a manner whilst always being aware that the cause of a facial asymmetry may not be as simple as it often seems.



