-
PDF
- Split View
-
Views
-
Cite
Cite
SG Mistry, BN Kumar, Balloon sinuplasty for an acute frontal sinus mucocele, Journal of Surgical Case Reports, Volume 2011, Issue 11, November 2011, Page 6, https://doi.org/10.1093/jscr/2011.11.6
Close - Share Icon Share
Abstract
Traditional management of mucoceles involve drainage using Functional Endoscopic Sinus Surgery (FESS) and if required an external approach. These techniques may dramatically alter the normal anatomy and function of the sinuses and are associated with significant complications. Balloon dilatation of the sinus ostia is a minimally invasive technique that has been licensed for use in chronic sinusitis. We report the use of this novel technique in the management of a frontal sinus mucocele in a 47-year old female. The frontal sinus was successfully cannulated, dilated and drained. The patient made a good post-operative recovery and remained asymptomatic at 6 months. We believe this to be a safe and effective technique for the management of mucoceles in the acute phase.
INTRODUCTION
A mucocele is defined as an “epithelial lined, mucus containing sac, that completely fills the sinus and is capable of expansion” (1).
This condition most commonly affects the fronto-ethmoidal region, with studies showing this involvement in up to 89% of patients with a mucocele (1). Disease of this region can result in symptoms such as pain, swelling, orbital displacement and visual disturbance.
The aetiology of this condition includes infection, polyps and trauma as predisposing factors. However, approximately one-third of all the cases have no obvious trigger.
Following medical management, surgical drainage is indicated with the use of functional endoscopic sinus surgery (FESS). For more complicated cases, a combined FESS and external approach has been commonly advocated. Serious complications such as haemorrhage, CSF leak and orbital damage have been reported for FESS with additional complications such as deformity and dural infections being reported for the external approach (1).
We describe the use of a new minimally invasive technique called balloon sinuplasty in the treatment of a frontal sinus mucocele.
CASE REPORT
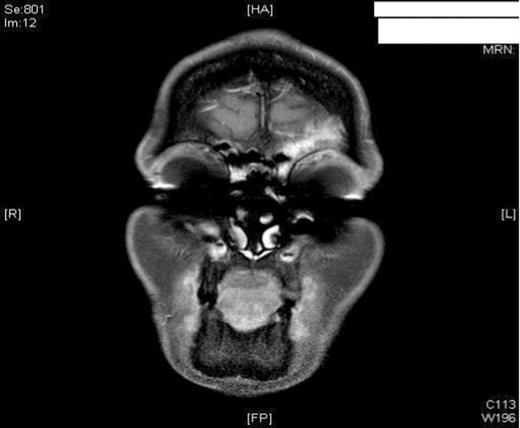
A 47-year old female smoker presented to the ENT department with worsening pain and progressive swelling to her left peri-orbital region and eyelid. On clinical examination the patient was acutely unwell. Rhinoscopy revealed mucopus draining from the left middle meatus. CT scanning revealed severe sinus disease in both frontal sinuses, with the left frontal sinus being expanded suggesting the presence of a mucocele (Figure 1). Both Frontonasal recesses and osteomeatal complexes were seen to be occupied by material bilaterally. Following Opthalmological review, she was managed initially with intravenous antibiotics and systemic steroids as well as intranasal steroids, decongestants and antimicrobial eye ointment. However, due to failure in resolution of symptoms, she was listed for surgical drainage of the mucocele using balloon sinuplasty.
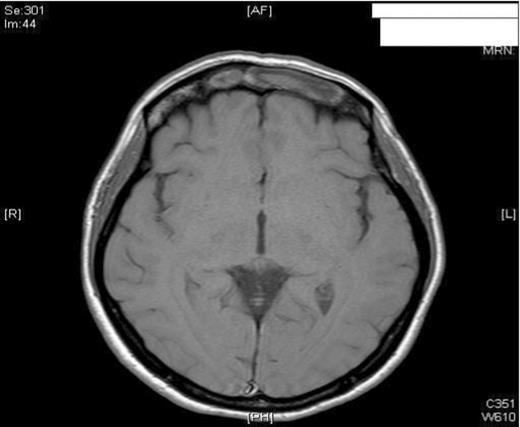
For our case, the patient was placed under general anaesthetic. Under endoscopic visualisation, a guidewire was passed within a catheter into the frontal sinus. The moment the guidewire passed into the recess there was a gush of mucopus and the forehead swelling gradually resolved. The position of this instrument was confirmed with trans-illumination – which was externally visible. Once in the correct position, a balloon was advanced over the guidewire and its position within the ostia verified using endoscopic visualisation. The balloon was subsequently inflated to 12 atmospheres pressure. Following this step, a large volume of mucopus was visualised draining from the ostium. An irrigation catheter was finally used to flush the sinus of any remaining mucopus and debris. Post- procedure, good ventilation of the ostia was visualised (Figure 2).
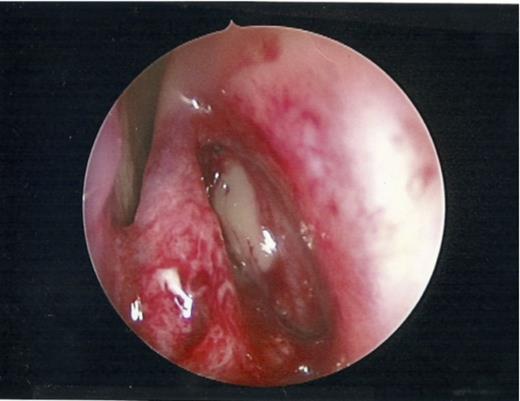
Patent ostia visualised endoscopically post dilatation with free drainage of mucopus.
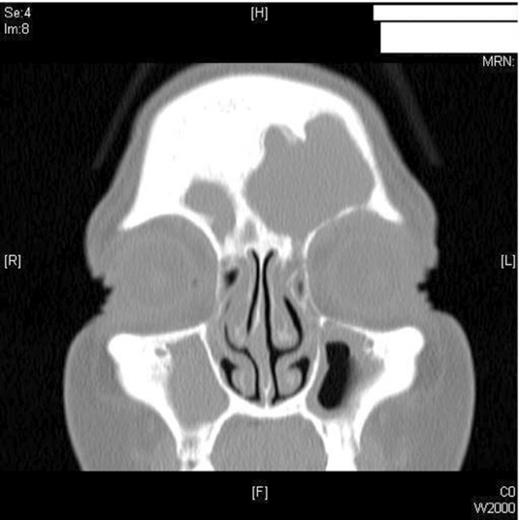
The patient had an uneventful post-operative period and remained pain-free with no residual swelling of the forehead. She was discharged home 24 hours post-operatively with FlixonaseTM Nasules for 6 weeks, SterimarTM spray for 2 months and regular steam inhalations. At 6 months post-op, the patient remained asymptomatic and well. To avoid any unnecessary radiation, the patient was assessed with MRI imaging. As shown, the imaging revealed no complications and showed adequate resolution of the mucocele (Figure 3).
MRI imaging (a) coronal (b) axial views post procedure revealing resolution of the mucocele and no intracranial or orbital complications (see figure 1).
DISCUSSION
Balloon dilatation has been successfully used in a number of medical and surgical specialties, for example, angioplasty for vascular patients. Such techniques gain popularity as a result of being minimally invasive which often leads to a shorter and less complicated post-operative period.
The use of balloon sinuplasty has almost exclusively been in the context of chronic rhinosinusitis(2). In 2009, Hopkins et al (3) described its use in the treatment of acute frontal sinusitis. They showed the technique to be safe and effective when used to drain an acutely infected frontal sinus. Although we describe the same technique as Hopkins et al, we have been able to show its effectiveness within a complication of sinsusitis not previously described, namely a mucocele.
As alluded to earlier, mucoceles are commonly managed by FESS and/or an external approach e.g. Lynch-Howarth frontoethmoidectomy or the osteoplastic flap procedure (Macbeths operation) (4). Such external techniques are necessary in cases where endoscopic marsupialisation is technically impossible to achieve due to anatomical and pathological factors (5). However, concerns regarding these techniques exist and relate to their complications such as frontal bossing/depression, CSF leak and infection (6). As a result, FESS has been championed with regard to its “less” invasive technique. Unfortunately, problems with FESS still exist especially in those where too much tissue removal has been performed to treat abnormal regions. This disruption to the normal anatomy and mucosa can have serious implications. For example, these patients may have recurrent or persistent disease, worsening or even new symptoms.
It has also been shown that FESS in frontal sinus surgery has higher failure rates as the procedure can be more technically difficult in comparison to other sinus surgery (7). This may be attributable to the complex and variable anatomy of the frontal recess. Therefore, balloon sinuplasty is an attractive intervention as it allows the operator to widen the natural ostia to allow for natural drainage rather than resecting the normal anatomy to achieve the result, thus avoiding serious complications. This was confirmed by the CLEAR (CLinical Evaluation to confirm safety and Efficacy in pARanasal sinuses) study which was a large multi-centred randomised study which reported no adverse effects and good efficacy up to 24-months (2).
We believe this to be the first reported case of the use balloon sinuplasty in the acute management of a frontal sinus mucocele. This may be attributable to the widespread use of FESS in this condition and the relatively low numbers of specialists trained in this technique. The overall aim in the management of mucoceles is to achieve drainage and to prevent recurrence as a result of obstruction. We have therefore shown that balloon sinuplasty has proved to be safe and effective in the short term. However, we are currently unsure whether any further procedures i.e. Lothrop’s operation are required to ensure long term patency of the ostia. Such information will only be available after long term follow-up and more widespread use of the procedure.
REFERENCES
The CLinical Evaluation to Confirm SAfety and Efficacy of Sinuplasty in the PaRanasal Sinuses (CLEAR) Study. Available at http://www.acclarent.com/clinical-education/clinical-data/clear-study/ Accessed 20 October 2010