-
PDF
- Split View
-
Views
-
Cite
Cite
PT Cheng, MM Ronald, GH Poole, Acute sleeve gastrectomy for a strangulated paraoesophageal hernia, Journal of Surgical Case Reports, Volume 2011, Issue 11, November 2011, Page 3, https://doi.org/10.1093/jscr/2011.11.3
Close - Share Icon Share
Abstract
Gastric necrosis in association with strangulation of a paraoesophageal hernia is a rare but life-threatening condition. The present article reports a case of strangulated paraoesophageal hernia with gastric necrosis in an obese woman treated successfully by acute sleeve gastrectomy.
INTRODUCTION
Most paraoesophageal hernias are asymptomatic and are discovered incidentally. Symptomatic cases need to be carefully assessed for risk/benefit when considering intervention. Occasionally the life-threatening complication of gastric volvulus, with or without strangulation, may present acutely. These cases are historically extremely complex to manage for the on-call surgeon. The technique described may help to simplify management.
CASE REPORT
A 73-year-old Caucasian woman presented to the emergency department with 2-day history of vomiting and vague abdominal pain. Her background history included asymptomatic hiatus hernia, morbid obesity (BMI of 35.7), polymyalgia rheumatica, previous laparoscopic cholecystectomy, hypercholesterolaemia and hypertension. Regular medications included prednisone, amlodipine and cilazapril. On presentation she was tachycardic at 110 beats/min with otherwise normal vital signs. Her abdomen was generally tender but without any localised peritonism. Initial laboratory investigations on admission showed a leukocytosis (WCC of 13.8 x 109/L). Routine X-ray (figure 1) and subsequent (CT) scan (figure 2) both revealed a large strangulated paraoesophageal hernia. Radiographic changes (figure 3) were seen with gas within stomach wall, suggestive of gastric necrosis.
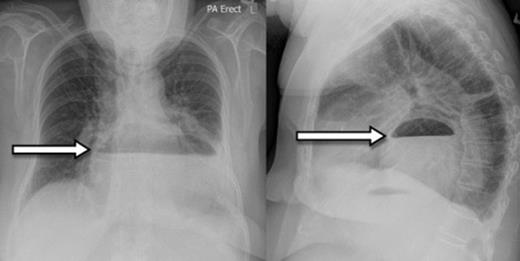
Chest X-ray showing paraoesophageal hernia with retro-cardiac air-fluid level (arrow)
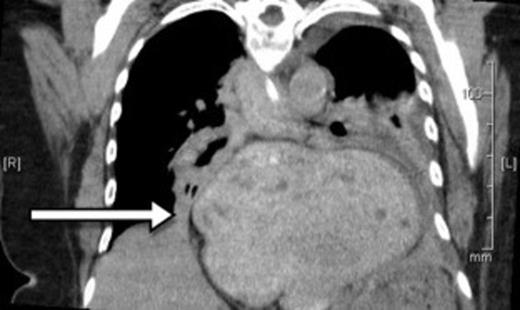
CT showing a large strangulated paraoesophageal hernia (arrow) within the thoracic cavity
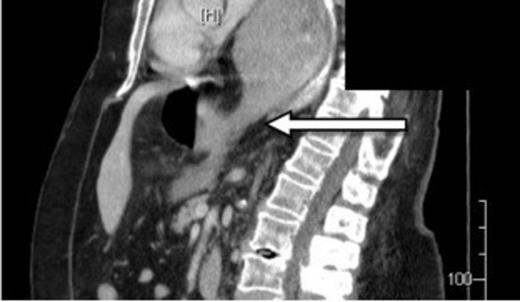
CT showing gas within stomach wall (arrow) suggestive of gastric necrosis
An urgent laparotomy was performed and a large paraoesophageal hernia was identified. The fundus and some of the greater curvature of stomach was necrotic but the lesser curvature had good blood supply. A formal sleeve gastrectomy was performed, calibrated upon a 34-F bougie, using a gastro-intestinal anastomosis (GIA) stapler and oversewn with 3/0 PDSTM (polyester polymer monofilament) sutures. A mesh was not placed and no attempt was made to repair the crura.
After 4 days in the high dependency ward she was transferred to the surgical ward. Soft pureed diet and proton pump inhibitor were commenced, and she was discharged 8 days later. One month follow-up reported almost full functional recovery with reduced gastric capacity and 8 kg of weight loss.
DISCUSSION
Paraoesophageal hernias occur when intra-abdominal contents prolapse through the diaphragmatic oesophageal hiatus, with maintenance of the normal infra-diaphragmatic location of the gastroesophageal junction. They form a small proportion of all hiatus hernias. There is a strong association between obesity and the incidence of paraoesophageal hernia(1). Some what surprisingly these hernias are often asymptomatic. Rarely, a life-threatening complication such as gastric volvulus, with or without strangulation, may occur(2). The estimated annual probability of a patient with a paraoesophageal hernia requiring emergency surgery is around 1%(3).
Traditionally, the goal of surgery is to remove the hernia sac and close the abnormally wide oesophageal hiatus(4). Some surgeons advocate gastropexy and fundoplication. Others also perform a temporary gastrostomy to help decompress stomach and provide some fixation(5). Obese patients have been noted to have high recurrence rates after all hiatus hernia repair(1). For this reason sleeve gastrectomy has been reported as a potentially useful alternative to gastropexy in the treatment of obese patients with gastroesophageal reflux with an associated hiatus hernia(6,7).
Our patient mandated an open approach with the aim to reduce strangulation of gastric volvulus and resection of necrotic organ. It was thought that sleeve gastrectomy could be an ideal option to treat both the gastric necrosis and the large paraoesophageal hernia, with the potential added benefit of weight loss in an obese patient. No attempt was made to repair the crura because this would have required the use of mesh which is problematic in the presence of a major contaminated resection.
Acutely strangulated paraoesophageal hernias represent real challenge in management for all on-call surgeons. Sleeve gastrectomy could be a useful surgical technique in managing acute complications of paraoesophageal hernia, especially in obese patients.



