-
PDF
- Split View
-
Views
-
Cite
Cite
Banan Muhsen Ali, Moatasem Hussein Al-janabi, Eiad Mansour, Ali Daoud, First documented case of decidualized endometriosis on the anterior peritoneum during emergency cesarean section: a case report and literature review, Journal of Surgical Case Reports, Volume 2025, Issue 9, September 2025, rjaf706, https://doi.org/10.1093/jscr/rjaf706
Close - Share Icon Share
Abstract
Endometriosis is a chronic gynecological condition characterized by the presence of endometrial-like tissue outside the uterine cavity. Although commonly associated with pelvic pain and infertility, its incidental discovery during a cesarean section is rare. To our knowledge, we report the first documented case of decidualized endometriosis identified on the anterior peritoneum during an emergency cesarean section in a 28-year-old woman with only one previous cesarean delivery and no prior symptoms. Histopathological examination confirmed the diagnosis, revealing significant decidual changes attributable to hormonal influences during pregnancy. This case highlights the importance of thorough intraoperative inspection, even during emergency procedures, as asymptomatic and atypically located endometriotic lesions can easily be overlooked. We discuss the clinical implications of this finding and provide a review of the relevant literature.
Introduction
Endometriosis affects ~10% of reproductive-aged women, manifesting with symptoms such as chronic pelvic pain, dysmenorrhea, and infertility [1, 2]. However, its discovery as an incidental finding during surgical procedures, particularly cesarean sections, is uncommon [3]. Decidualization, a physiological process during pregnancy, may obscure or modify typical endometriotic lesions, posing diagnostic challenges [4]. This case report details a unique presentation of decidualized endometriosis identified during an emergency cesarean section and underscores the importance of histopathological evaluation in such scenarios.
Case presentation
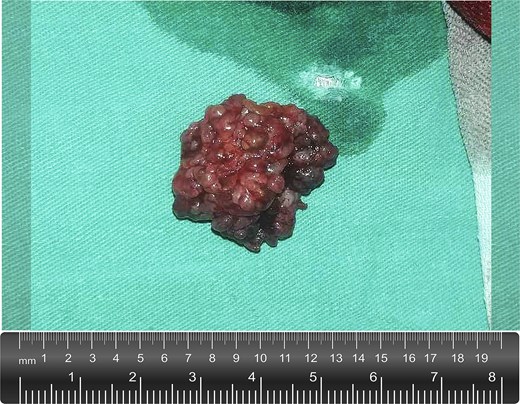
A 28-year-old woman, gravida 2 para 1, presented to our university hospital in active labor at 37 weeks of gestation, with clinical and radiological evidence of cephalopelvic disproportion and non-reassuring fetal status. An emergency cesarean section was performed. During abdominal closure, intraoperative assessment revealed a firm, irregular, yellowish-brown nodule measuring ~2.5 cm on the anterior peritoneum, distant from the uterine incision site and unrelated to the operative field. The lesion appeared well-circumscribed, superficial, and without signs of invasion or adhesions (Fig. 1; Supplementary Video S1). Given its uncertain nature and to exclude malignancy, it was excised in toto and sent for histopathological evaluation. The procedure was completed without complications, adding ~10 minutes to the operative time.

Intraoperative image showing a firm, irregular, nodular lesion measuring ~2.5–3 cm on the anterior peritoneal surface. The lesion has a reddish-brown appearance and is being carefully excised using surgical forceps and scissors. It was incidentally discovered during abdominal closure in an emergency cesarean section, unrelated to the surgical field or previous scar site.
Grossly, the excised lesion measured ~2 × 3 cm and appeared as an irregular, lobulated mass with a grayish-red external surface. It was of moderate to firm consistency, and the cut surface was lobulated and whitish (Fig. 2). Microscopic examination revealed ectopic endometrial glands surrounded by decidualized stroma. The stromal cells were large, polygonal, with abundant eosinophilic cytoplasm and centrally located round nuclei, consistent with pregnancy-related decidualization (Fig. 3). No cytological atypia, abnormal nuclear features, or mitotic figures were identified. The overlying peritoneum was intact, confirming the lesion’s superficial location. Immunohistochemical staining for CD10—a sensitive and well-established marker of endometrial stroma—was performed to confirm the diagnosis. The stromal cells exhibited strong and diffuse cytoplasmic positivity (Fig. 4), supporting the final diagnosis of decidualized endometriosis.
Gross appearance of the excised lesion. The mass measured ~2 × 3 cm, with an irregular, lobulated contour and a grayish-red external surface. It was of moderate to firm consistency. The cut surface revealed a lobulated, whitish appearance.
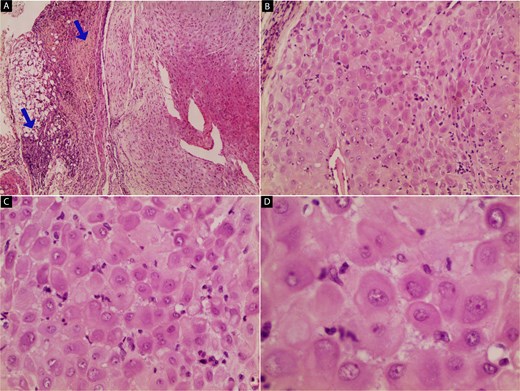
Histopathological features of the excised lesion (hematoxylin and eosin stain): (A) low-power view showing decidualized endometrial stroma with adjacent endometrial glands; blue arrows indicate the overlying peritoneal tissue (40×). (B) Intermediate magnification revealing decidualized stromal cells with abundant eosinophilic cytoplasm and centrally located nuclei, consistent with pregnancy-related changes (100×). (C) High-power view showing uniform polygonal decidualized stromal cells without cytological atypia or malignancy (200×). (D) Close-up of decidualized stroma highlighting the prominent, round nuclei and abundant cytoplasm, confirming the benign nature of the lesion (400×).
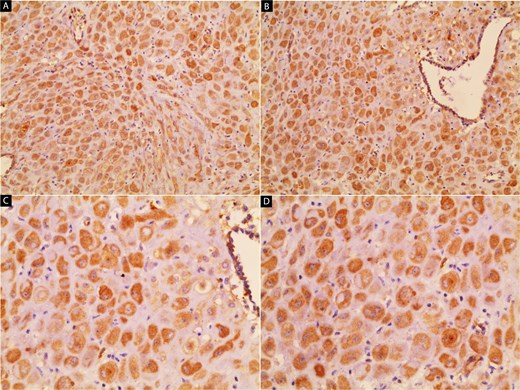
Immunohistochemical staining for CD10. The stromal component of the lesion shows strong, diffuse cytoplasmic positivity, confirming its endometrial stromal origin and supporting the diagnosis of decidualized endometriosis. Images (A) and (B) show 100× and 200× magnifications, respectively.
The patient’s history revealed a cesarean delivery 18 months previously with no symptoms of endometriosis (cyclic pelvic pain, dysmenorrhea, or infertility) at any time before presentation, and the lesion was undetected on multiple prenatal ultrasounds. The patient’s postoperative course was uneventful. On postoperative Day 1, she tolerated an oral diet and ambulated without assistance. She was discharged home in stable condition on Day 2. At the 6-week postpartum visit, the surgical wound had completely healed, with no signs of infection. She denied abdominal pain, abnormal bleeding, or any other complaints, and had resumed normal daily activities. At a 3-month telephone follow-up, she remained asymptomatic with no clinical suspicion of recurrence.
Discussion
Endometriosis is a chronic gynecological condition characterized by the presence of endometrial-like tissue outside the uterine cavity, affecting ~10% of women of reproductive age [1, 2]. While commonly associated with pelvic pain and infertility, its incidental discovery during a cesarean section is rare [3].
Decidualized endometriosis (DE) occurs due to elevated progesterone levels during pregnancy, leading to significant morphological changes in ectopic endometrial tissue [4]. These changes can obscure typical lesions, posing diagnostic challenges [5]. Decidualization is characterized by the enlargement of stromal cells, increased vascularization, and a robust secretory phenotype [6]. In the context of endometriosis, these changes may mimic malignancy or inflammatory lesions, making histopathological evaluation crucial [7].
The anterior peritoneal surface is an unusual location for DE, as most reported cases are found on the ovaries, uterine serosa, or cesarean scars [8]. To our knowledge, we report the first documented case of clinically silent DE discovered on the anterior peritoneum during an emergency cesarean section in a 28-year-old woman with only one prior cesarean delivery and no previous symptoms. Notably, the lesion was situated away from the cesarean scar. A review of the literature reveals that the incidence of decidualized endometriosis during cesarean sections is likely underreported [9], possibly due to its asymptomatic nature and the lack of routine histopathological analysis of incidental lesions [10]. Increased documentation and reporting of such cases are essential to enhance our understanding of the condition and its clinical implications [11].
The incidental finding highlights the importance of thorough intraoperative examination of the peritoneal surfaces, even during emergency procedures.
During surgery, intraoperative differentials for such a lesion may include peritoneal metastases, tuberculous peritonitis, granulomatous inflammation, or benign reactive processes such as fibrous adhesions or scar nodules. Recognizing decidualized endometriosis among these possibilities is essential to avoid unnecessary extensive resections or staging procedures [9, 10]. From a surgical relevance perspective, identifying and excising suspicious lesions at the time of cesarean delivery provides both diagnostic clarity and potential symptom prevention. In our case, excision was straightforward, added minimal operative time, and avoided the need for reoperation or delayed diagnosis. Such proactive management can be particularly important in resource-limited settings where postoperative follow-up may be inconsistent [12, 13].
Furthermore, the presence of decidualized endometriosis highlights the need for heightened awareness among obstetric surgeons and pathologists [14]. Misinterpreting such lesions as malignancies could lead to overtreatment or unnecessary patient anxiety. This underscores the importance of distinguishing decidualized endometriosis from other peritoneal abnormalities using advanced diagnostic techniques, including immunohistochemistry and molecular profiling [15].
Management of incidental endometriosis discovered during cesarean section remains individualized [12]. For asymptomatic patients, no additional surgical intervention is typically required. However, patients with a history of endometriosis or symptoms suggestive of its presence may benefit from postoperative follow-up and counseling [10]. The impact of pregnancy on the progression or regression of endometriosis is variable and depends on factors such as lesion location, hormonal milieu, and patient-specific immune responses [13].
This case contributes to the growing body of evidence suggesting that decidualized endometriosis, though rare, is an important differential diagnosis for peritoneal lesions observed during pregnancy. It also raises questions about the potential long-term implications of pregnancy-induced decidualization on the progression or resolution of endometriotic lesions.
Conclusion
The incidental discovery of decidualized endometriosis during cesarean section underscores the importance of careful intraoperative inspection and histopathological evaluation. While rare, such findings provide valuable insights into the behavior of endometriosis during pregnancy and inform postoperative care strategies. Further studies are needed to elucidate the clinical significance and long-term implications of decidualized endometriosis.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Funding
None declared.
Ethical approval
No ethical approval is required for this case report.
Guarantor
Moatasem Hussein Al-janabi.
Consent
Informed and written consent from the patient was taken prior to publication.



