-
PDF
- Split View
-
Views
-
Cite
Cite
Yassine El Bouazizi, Amine El Bouazizi, Sabrillah Echiguer, Taha Kabbaj, Zakaria El Mouatassim, Oumaima Lahnaoui, Amine Souadka, Mohammed Anass Majbar, Amine Benkabbou, Hepatomesenteric trunk: a rare variant with major surgical implications. A case report from a living donor for liver transplantation, Journal of Surgical Case Reports, Volume 2025, Issue 7, July 2025, rjaf499, https://doi.org/10.1093/jscr/rjaf499
Close - Share Icon Share
Abstract
Anatomical variations of the hepatic artery are common, with the most frequent being the right hepatic artery arising from the superior mesenteric artery, described as Michels type III. A rarer variant, the hepatomesenteric trunk, occurs when both the common hepatic artery and superior mesenteric artery share a common origin from the abdominal aorta. This variation, classified as Michels type IX and Adachi type V, presents significant implications for hepatobiliary and pancreatic surgery, as well as liver transplantation. We report a case of a 27-year-old female living donor for liver transplantation, whose preoperative imaging revealed a hepatomesenteric trunk. This rare variant required careful surgical planning, especially in the context of liver donor hepatectomy. The recognition of such variations is crucial for preventing inadvertent vascular injury and ensuring optimal graft perfusion. The case highlights the importance of preoperative vascular imaging and tailored surgical strategies in managing complex vascular anatomies.
Introduction
Variants of hepatic arterial anatomy are common, occurring in 20% to 30% of cases [1]. Michels’ classification describes the main variants, the most common being the right hepatic artery originating from the superior mesenteric artery (SMA), known as type III. Type IX, which is rarer (1% to 3% of cases), corresponds to the origin of the common hepatic artery (CHA) from the SMA [1]. In certain configurations, the CHA and the SMA share a common trunk, forming a hepatomesenteric trunk, while the celiac trunk only gives rise to the left gastric artery and the splenic artery, thus forming a gastrosplenic trunk [2–4]. This arrangement, classified as Adachi type V, is extremely rare and can present major technical challenges in hepatobiliary, pancreatic surgery, and particularly in liver transplantation.
Case presentation
A 27-year-old woman, with no notable medical history, was evaluated as a living donor for her 9-year-old son with hepatic failure. The preoperative workup included an abdominal-pelvic CT angiogram and a biliary MRI. The biliary MRI showed normal biliary ducts. However, the CT angiogram revealed a significant vascular variation: the absence of the typical celiac trifurcation (Figs 1 and 2). The celiac trunk gave rise only to the left gastric artery and the splenic artery, forming a gastrosplenic trunk, while a second arterial trunk originating from the abdominal aorta at the level of L1 simultaneously gave rise to the SMA and the CHA: a hepatomesenteric trunk.
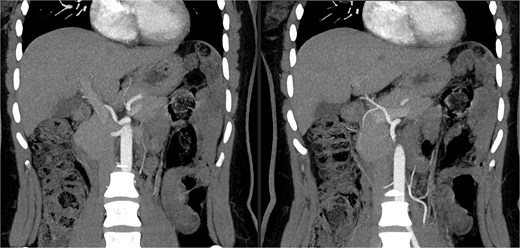
CT angiogram showing the celiac trunk giving rise to the left gastric artery and splenic artery, along with the hepatomesenteric trunk.

3D reconstruction using Myrian software illustrating the arterial anatomical variation.
The CHA then divided into the right and left hepatic arteries, ensuring normal hepatic perfusion. No other pathological findings were identified. The patient was asymptomatic. This finding did not contraindicate liver donation but required a reevaluation of the surgical strategy.
Discussion
Frequency and anatomy
Variations of the CHA are well described by Michels, whose classification remains a reference [1]. The origin of the CHA from the SMA, as in our case, is designated as type IX. The presence of a hepatomesenteric trunk, associated with a reduced celiac trunk giving rise to a gastrosplenic trunk, is extremely rare: it is observed in ~0.5% to 1% of cases according to several studies [3–5]. Choi et al. reported this variation in <0.5% of cases in a study of over 5000 patients [4]. Kahraman et al. and Kardile and Majale reported isolated cases during anatomical dissections [2, 3].
Implications in pancreatic surgery
In the context of a pancreaticoduodenectomy, this variation requires particular attention. The presence of a hepatomesenteric trunk necessitates careful dissection around the SMA from the beginning of the procedure, in what is known as the SMA-first approach [6, 7]. In the absence of preoperative identification, accidental injury to the CHA may occur, leading to severe hepatic ischemia and increased morbidity. In case of injury, vascular reconstruction can be considered, either by direct suturing or with an interposition graft [6].
Implications in liver transplantation
In living donor liver transplantation, particularly for left lobe procurement, the presence of a hepatomesenteric trunk complicates arterial dissection. Since the left hepatic artery originates from this trunk, it is often necessary to harvest a long arterial segment, sometimes with interposition of a graft, to facilitate the anastomosis in the recipient [7, 8].
Maintaining optimal perfusion of the residual liver (right lobe) in the donor requires precise dissection of the bifurcation of the CHA. In our case, this bifurcation occurred after the CHA left the hepatomesenteric trunk, allowing preservation of right vascularization.
Moreover, vascular complications are one of the leading causes of early graft loss in liver transplantation. Inadequate vascular reconstruction may lead to thrombosis, stenosis, or postoperative hemorrhage [9].
Importance of preoperative imaging
Erbay et al. demonstrated that >60% of living donors have at least one significant vascular variation, highlighting the importance of a preoperative CT angiogram with 3D reconstruction [5]. This imaging technique allows for precise mapping of the vascular tree, which is essential for surgical planning. In our case, this planning enabled the adaptation of the harvesting technique, ensuring the safety of both the donor and the recipient.
Conclusion
This case illustrates a rare but important variant of hepatic arterial vascularization: the hepatomesenteric trunk associated with a gastrosplenic trunk, corresponding to Michels type IX and Adachi type V. Its recognition is critical in hepatobiliary and pancreatic surgery, and especially in living donor liver transplantation. Careful vascular exploration allows for the anticipation of technical challenges, ensures safe dissection, and avoids severe complications. While complex, this variant does not contraindicate liver donation if an appropriate surgical strategy is employed.
Conflict of interest statement
The authors declare that they have no conflict of interest.
Funding
None declared.
Informed consent
Patient consented to the submission of their case reports and the use of their personal pictures to this submission.



