-
PDF
- Split View
-
Views
-
Cite
Cite
Meaad K Alsulami, Aljawharah A Alotaibi, Alaa O Jamjoom, Rare case of non-Hodgkin lymphoma of the appendix and ileocecal valve presenting as acute perforated appendicitis, Journal of Surgical Case Reports, Volume 2025, Issue 5, May 2025, rjaf274, https://doi.org/10.1093/jscr/rjaf274
Close - Share Icon Share
Abstract
Non-Hodgkin lymphoma of the gastrointestinal tract is one of the least common primary malignancies, with diffuse large B-cell lymphoma being the most common histological subtype. Primary appendiceal lymphoma is extremely rare, with symptoms usually mimicking those of acute appendicitis. Here, we present a rare case of primary appendiceal non-Hodgkin lymphoma with ileocecal valve involvement and coexistence of Schistosoma eggs. The patient was initially diagnosed with acute perforation appendicitis. Following laparoscopic appendectomy, the patient developed an enterocutaneous fistula, which was addressed surgically after the failure of conservative management. Adjuvant chemotherapy with R-CHOP regimen was further planned for the patient.
Introduction
Primary lymphoma of the appendix is exceedingly rare and is found in approximately 0.013% of all appendectomy specimens [1]. Appendiceal non-Hodgkin lymphoma (NHL) often presents with non-specific symptoms and may present with symptoms of acute appendicitis. Consequently, a definitive diagnosis of appendiceal NHL is usually made postoperatively upon histopathological examination.
Only a few cases of appendiceal NHL are reported in the literature [2]. Here, we present the case of a 26-year-old male with NHL involving the appendix and ileocecal valve who initially presented with acute perforated appendicitis. To the best of our knowledge, and upon extensive review of the literature, this report represents the first reported case of NHL involving such a unique area as the ileocecal valve together with the appendix, with identification of Schistosoma eggs in the specimen.
Case report
A 26-year-old male patient presented with a 3-day history of severe lower abdominal pain. The pain was localized in the right lower quadrant on the day of presentation. It was sharp, continuous, and aggravated with movement. The patient had never experienced any similar pain attacks. He had a history of fever, nausea, vomiting, and watery diarrhea. The patient denied weight loss, family history of malignancy, or any drug history. He had a history of schistosomiasis during childhood and had received treatment. Otherwise, the patient was medically free.
Abdominal computed tomography (CT) revealed a dilated appendix filled with fluid, measuring 2.7 × 8 cm on the short and long axes, respectively, with significant surrounding fat stranding, free fluid, and reactive inflammatory changes involving the terminal ileum and cecum, along with a few prominently enlarged regional lymph nodes (Fig. 1). Other investigations revealed a hemoglobin level of 12.6 g/dL, white blood cell count of 11.3 × 109/L with an absolute neutrophil count of 10.3 × 109/L, and erythrocyte sedimentation rate of 64 mm/h.

Axial view of abdominal and pelvic CT scan with oral and IV contrast shows enlarged appendix, measured 2.7 in diameter. Surrounded by fat-stranding, free fluid, with enlarged reactive lymph nodes (arrow).
Therefore, the patient was admitted with the impression of acute complicated appendicitis, and appropriate antibiotic therapy was initiated. Laparoscopic appendectomy was planned for the patient. Intraoperatively, the appendix was dilated, filled with thick fluid, and severely inflamed, with adhesions and perforation at the base. Due to the severe adhesions encountered, the procedure was converted to an open low-midline laparotomy, and ileocecal resection was performed with primary anastomosis. On the third postoperative day, the patient was discharged in a good condition.
One week after surgery, the patient developed a surgical site infection with the development of a low-output enterocutaneous fistula (Fig. 2). The patient was treated conservatively with subcutaneous abscess drainage, antibiotics, diet modification, and wound care.

Sagittal view of abdominal and pelvic CT scan with IV and oral contrast shows anterior abdominal wall collection near the supra-umbilical wound with faint linear contrast within the collection representing enterocutaneous fistula.
The histopathology report reviewed at the time revealed the presence of a mass in the ileocecal valve extending to the appendiceal orifice, measuring 4 × 4 × 3 cm, with clear proximal and distal resection margins. The tumor was identified as a diffuse large B-cell lymphoma (DLBCL) of germinal center derivation. It was positive for CD45 (variable), CD20, BCL6, and CD10 and negative for MUM1, BCL2, and c-MYC (control weak); the ki-67 proliferative index was very high at 95%. Tumor cells were identified in the appendix by the extension of the ileocecal valve. Secondary transmural necrotizing appendicitis was also observed. Three reactive lymph nodes were identified and Schistosoma ova were identified in the appendix (Fig. 3). Molecular tests returned normal results for the genes MYC, BCL2, and BCL6.
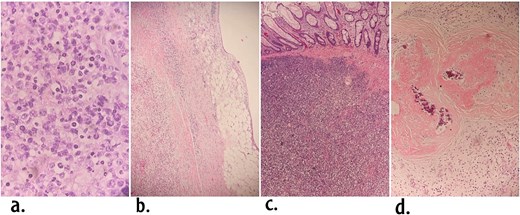
Histological features of the tumor. (a) The mucosa is diffusely infiltrated with medium sized lymphoid cells with round nuclei in the area of ileocecal valve (Hematoxylin and eosin ×40). (b) DLBCL in the appendiceal wall. (c) DLBCL in the ileocecal valve area underneath intact mucosa. (d) Calcified Schistosoma eggs in the appendix.
To complete the metastatic workup, CT scans of the neck, chest, abdomen, and pelvis were performed, which showed no metastatic deposits or lymphadenopathy. A medical oncology opinion was obtained and adjuvant chemotherapy (R-CHOP regimen) was planned.
Discussion
Enterocutaneous fistula is a complication that can occur postoperatively or after chemotherapy. Our patient, who presented day 10 postoperative with CT findings of an enterocutaneous fistula, was treated with antibiotics because the output was low. Subsequently, the patient was referred to an oncology center to initiate adjuvant therapy. However, after two sessions of the R-CHOP regimen, the patient complained of increased fistula output and abdominal pain. The patient’s condition was optimized with total parenteral nutrition, after which he underwent successful fistula closure surgery and was referred to the oncology department to resume chemotherapy.
Prognosis and survival depend on many factors, including cancer stage and grade and patient’s age and overall health. The overall survival (OS) of patients diagnosed with primary appendiceal lymphoma is 185 months, with a 5-year survival rate of 67%. No statistically significant difference in OS has been observed between sexes, races, or histological subtypes. However, an increased age at diagnosis has been associated with an increased risk of death [3].
Schistosomiasis, also known as bilharziasis, is one of the most common infectious parasitic diseases globally. It is caused by blood trematodes or flukes belonging to the genus Schistosoma. The three main species that infect humans are Schistosoma haematobium, Schistosoma japonicum, and Schistosoma mansoni.
Of these, S. haematobium has been linked to squamous cell carcinoma of the bladder and is classified as a Group 1 carcinogen [4]. In contrast, S. mansoni has been implicated in multiple types of cancers in various case reports and series. These include hepatocellular carcinoma [1, 5, 6], colorectal cancer [7, 8], bladder carcinoma [9], and prostate cancer [10]. The association between NHL and S. mansoni was investigated by Andrade [11], who studied 863 cases of splenectomy for follicular lymphoma of the spleen and found that approximately 1% of the cases were associated with hepatosplenic schistosomiasis.
In our case, the patient reported a history of schistosomiasis and was successfully treated. Histopathological examination of the appendix revealed the presence of Schistosoma ova. Because NHL is the least frequent type of cancer affecting the appendix, the coexistence of Schistosoma ova in the appendix alongside NHL cells was not considered coincidental. To the best of our knowledge, this observation has never been reported in the existing literature, and this is probably the first such case, raising questions about the possible associations between them.
Conflict of interest statement
None declared.
Funding
None declared.



