-
PDF
- Split View
-
Views
-
Cite
Cite
Brent Llera, Iman Hanna, Michael Jureller, Eosinophilic appendicitis: an insidious and fortuitous diagnosis, Journal of Surgical Case Reports, Volume 2024, Issue 6, June 2024, rjae380, https://doi.org/10.1093/jscr/rjae380
Close - Share Icon Share
Abstract
Eosinophilic appendicitis is a rare inflammatory condition characterized by the infiltration of eosinophils into the appendix, which is often misdiagnosed as acute appendicitis given similarities in their clinical presentation. Acute eosinophilic appendicitis: a rare cause of lower gastrointestinal hemorrhage. Within this particular report, we present a case of eosinophilic appendicitis in a 42-year-old female who underwent a laparoscopic appendectomy. The purpose of this report is to increase awareness about this unique condition and emphasize the importance of considering eosinophilic appendicitis as a differential diagnosis in patients with appendicitis-like symptoms whose clinical examination and laboratory findings may suggest otherwise.
Introduction
Appendicitis is a common surgical emergency where inflammation of the organ manifests from obstruction of the appendiceal lumen, which may result from an appendicolith or other mechanical etiology. As such, this obstruction results in generalized inflammation of the appendix with a subsequent build-up of viral, bacterial, or even parasitic organisms. With that in mind, several other conditions can mimic acute appendicitis, leading to a myriad of diagnostic challenges. For example, eosinophilic appendicitis, characterized by eosinophilic infiltration of the appendix wall, is a rare entity that can mimic acute appendicitis clinically [1, 2]. Therefore, it is important to distinguish eosinophilic appendicitis from other causes of right lower quadrant abdominal pain so as to provide appropriate management and avoid conducting unnecessary surgery.
Case presentation
A 42-year-old female with a past medical history significant for gluten intolerance and seasonal allergies presented to the emergency department with a three-day history of right lower quadrant abdominal pain and poor appetite in conjunction with reported fevers at home as high as 38.6°C. The pain was progressively worsening and associated with non-bloody, non-bilious emesis on three occasions. On examination, there was tenderness in the right lower quadrant, with localized guarding and rebound tenderness at McBurney’s point. Laboratory investigations revealed a normal white blood cell count (4900/μl) without a left shift or eosinophilia. A computed tomography (CT) scan (Fig. 1), showed an 8 mm dilated appendix with peri-appendiceal fat stranding, suggestive of acute appendicitis.
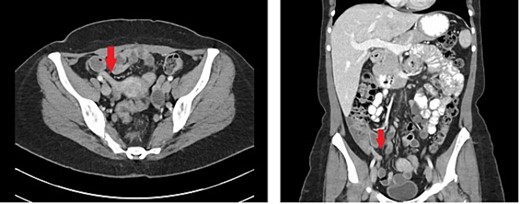
Representative axial and coronal cuts of CT imaging showing an 8 mm dilated appendix noted by the arrow.
Based on the clinical and radiological findings, a diagnosis of acute appendicitis was made, and the patient underwent an urgent laparoscopic appendectomy. Intraoperatively, the appendix appeared full and not significantly inflamed nor edematous. Histopathological examination of the resected appendix revealed transmural infiltration of eosinophils, with no evidence of granuloma formation or parasites. These findings were consistent with eosinophilic appendicitis.
Postoperatively, her presenting pain resolved, and she was discharged from recovery. She was later seen in the outpatient setting and has recovered uneventfully.
Discussion
Eosinophilic appendicitis is a rare condition that can present similarly to acute appendicitis. The exact etiology of eosinophilic appendicitis continues to remain unclear; however, it is thought to be related to an allergic or immunological response [3]. It can occur in isolation or as part of a systemic eosinophilic disorder, such as eosinophilic gastroenteritis or esophagitis. The clinical presentation, laboratory findings, and imaging studies in eosinophilic appendicitis can mimic acute appendicitis, making it difficult to differentiate the two preoperatively.
Histopathological examination is crucial in confirming the diagnosis of eosinophilic appendicitis. Characteristic findings include eosinophilic infiltration of the appendix wall, absence of granuloma formation or parasites, and exclusion of other causes of eosinophilia, such as malignancy [3, 4]. As noted in the images below, the mucosa of appendix can be seen with a mild eosinophilic infiltrate of the lamina propria and rare intraepithelial eosinophils (Fig. 2A), as well scattered eosinophils throughout the muscularis propria (Fig. 2B and C). In any event, the management of eosinophilic appendicitis involves surgical intervention with appendectomy, similar to acute appendicitis given a majority of patient’s initial presentation within the acute setting [2, 5].
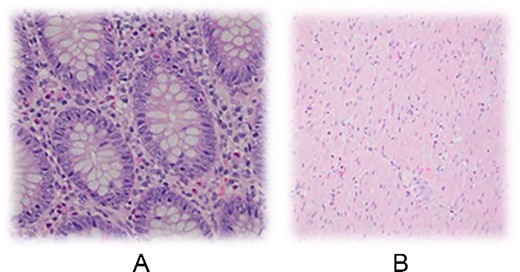
Mucosa of appendix can be seen with a mild eosinophilic infiltrate of the lamina propria and rare intraepithelial eosinophils. B Scattered eosinophils throughout the muscularis propria.
Conclusion
Eosinophilic appendicitis is a rare condition that can mimic acute appendicitis clinically. It is important for clinicians to be aware of this entity and consider it as a differential diagnosis in patients presenting with appendicitis-like symptoms. Histopathological examination is necessary to confirm the diagnosis. Further research is needed to better understand the pathogenesis and optimal management of eosinophilic appendicitis.
Acknowledgements
The author(s) thank NYU Langone Hospital Long Island for providing the imaging and reports utilized within this case report.
Author contributions
B.L. made literature search, manuscript writing, design and image providing.M.J. contributed to literature search, case writing and image providing.I.H. contributed to pathology reports, histology reports, and image providing.All the authors (B.L., M.J., and I.H.) revised the manuscript and agreed on its conclusions.
Conflict of interest
This article has not been presented nor published elsewhere, and no financial support has been obtained in its preparation. In addition, the patient has provided written consent to the publication of the case report and pictures.
Funding
None.



