-
PDF
- Split View
-
Views
-
Cite
Cite
Bassam Adel Shawasha, Asala M Awaysa, Mohammad I Smerat, Sulaiman Naji Fares Fakhouri, Traumatic appendicitis with mass formation, a rare case report, Journal of Surgical Case Reports, Volume 2024, Issue 4, April 2024, rjae265, https://doi.org/10.1093/jscr/rjae265
Close - Share Icon Share
Abstract
This case report delves into an atypical presentation of postblunt abdominal trauma in an adult male, characterized by acute appendicitis complicated by the formation of an appendicular inflammatory mass. The patient’s clinical evolution, diagnostic intricacies, and the multidisciplinary approach employed for successful management. By documenting this rare complication, our report contributes to expanding knowledge base on unusual consequences of abdominal trauma, aiming to enhance awareness and facilitate informed decision-making in clinical practice.
Introduction
Blunt abdominal trauma often gives rise to a spectrum of injuries, ranging from common presentations to rare and intricate complications. This case report explores an unusual consequence of such trauma in an adult male patient: acute appendicitis with mass formation extending into the urinary bladder. Although acute appendicitis is a well-known entity, its coexistence with an inflammatory mass involving the bladder following blunt abdominal trauma is a rare occurrence. The complexity of this case necessitates a thorough examination of the patient’s clinical history, diagnostic challenges, and the tailored approach undertaken for successful management. By presenting this distinctive case, we aim to contribute valuable insights to the medical community, enhancing our understanding of the diverse sequelae that may arise in the aftermath of blunt abdominal trauma.
Case presentation
A 28-year-old male patient with free past history presented to our department after experiencing vague abdominal and bilateral flank pain for 2 weeks. The pain radiates to the groin region and associated with decreased appetite and urinary symptoms. The onset of pain started 3 days after the patient experienced blunt abdominal trauma after falling from ∼2 m height, hitting his knee against his abdomen. There is no history of fever, vomiting, or changes in bowel habits. The patient sought medical advice at an outpatient clinic in his town, where complete blood testing and urine analysis showed leukocytosis and a mild urinary tract infection. C-reactive protein was positive at 12 mg/l, while alanine transaminase (22) and t bilirubin (0.5) were normal.
Patient was treated as urinary tract infection (UTI) but showed no improvement.
After that his pain increased in severity and he developed a spike of fever, prompting him to seek medical advice at our hospital. Upon examination, he appeared ill, pale, in pain, with signs of dehydration. His vital signs showed tachycardia with a heart rate of 123 beats per minute and hypotension with a blood pressure of 96/59. He was not in respiratory distress, and his SpO2 was: 96%, with increased capillary refill time: 4–5 s. Upon abdominal examination, his abdomen was rigid and guarding with diffuse tenderness maximumly at right iliac fossa, otherwise unremarkable.
Laboratory tests showed leukocytosis in the blood, and urine microscopy showed hematuria and leukocyturia. Serum creatinine was elevated mostly due to dehydration and then normalized after rehydration and appropriate management. Serum electrolytes showed mild hyponatremia and otherwise unremarkable. Hepatitis profile was negative, and his other routine labs are unremarkable (Tables 1–5).
| CBC . | . | . |
|---|---|---|
| Normal range | Result | Test |
| 4.6–11 K/Ul | 30.6 | WBCs |
| 3%–7% | 3.4 | Monocytes % |
| 0%–0.75% | 0.5 | Basophils % |
| 37%–92% | 92.2* | Neutrophils granulocytes % |
| - % | 2.8 | Lymphocytes % |
| 4.69–6.13 M/Ul | 6 | RBCs |
| 13.5–17 g/dl | 17.3 | Hemoglobin |
| 43.5%–53.7% | 52 | Hematocrit |
| 80–100 fl | 86.7 | (MCV) |
| 150–450 K/μl | 470* | Platelets count |
| CRP | 254.1 | 0–5 |
| CBC . | . | . |
|---|---|---|
| Normal range | Result | Test |
| 4.6–11 K/Ul | 30.6 | WBCs |
| 3%–7% | 3.4 | Monocytes % |
| 0%–0.75% | 0.5 | Basophils % |
| 37%–92% | 92.2* | Neutrophils granulocytes % |
| - % | 2.8 | Lymphocytes % |
| 4.69–6.13 M/Ul | 6 | RBCs |
| 13.5–17 g/dl | 17.3 | Hemoglobin |
| 43.5%–53.7% | 52 | Hematocrit |
| 80–100 fl | 86.7 | (MCV) |
| 150–450 K/μl | 470* | Platelets count |
| CRP | 254.1 | 0–5 |
| CBC . | . | . |
|---|---|---|
| Normal range | Result | Test |
| 4.6–11 K/Ul | 30.6 | WBCs |
| 3%–7% | 3.4 | Monocytes % |
| 0%–0.75% | 0.5 | Basophils % |
| 37%–92% | 92.2* | Neutrophils granulocytes % |
| - % | 2.8 | Lymphocytes % |
| 4.69–6.13 M/Ul | 6 | RBCs |
| 13.5–17 g/dl | 17.3 | Hemoglobin |
| 43.5%–53.7% | 52 | Hematocrit |
| 80–100 fl | 86.7 | (MCV) |
| 150–450 K/μl | 470* | Platelets count |
| CRP | 254.1 | 0–5 |
| CBC . | . | . |
|---|---|---|
| Normal range | Result | Test |
| 4.6–11 K/Ul | 30.6 | WBCs |
| 3%–7% | 3.4 | Monocytes % |
| 0%–0.75% | 0.5 | Basophils % |
| 37%–92% | 92.2* | Neutrophils granulocytes % |
| - % | 2.8 | Lymphocytes % |
| 4.69–6.13 M/Ul | 6 | RBCs |
| 13.5–17 g/dl | 17.3 | Hemoglobin |
| 43.5%–53.7% | 52 | Hematocrit |
| 80–100 fl | 86.7 | (MCV) |
| 150–450 K/μl | 470* | Platelets count |
| CRP | 254.1 | 0–5 |
| Test . | Result . | Normal range . |
|---|---|---|
| INR | 1.88 | |
| PT | 23.5 | 11–15 |
| PTT | 29.5 | 25–35 |
| Test . | Result . | Normal range . |
|---|---|---|
| INR | 1.88 | |
| PT | 23.5 | 11–15 |
| PTT | 29.5 | 25–35 |
| Test . | Result . | Normal range . |
|---|---|---|
| INR | 1.88 | |
| PT | 23.5 | 11–15 |
| PTT | 29.5 | 25–35 |
| Test . | Result . | Normal range . |
|---|---|---|
| INR | 1.88 | |
| PT | 23.5 | 11–15 |
| PTT | 29.5 | 25–35 |
| Test . | Result . | Normal range . |
|---|---|---|
| ALT | 12 | 0–41 |
| S. CREATININE | 2.18 | 0.7–1.2 |
| BUN | 12 | 6–20 |
| S. amylase | 55 | 28–100 |
| S. Sodium | 133 | 135–145 |
| S. Potassium | 4.4 | 3.5–5.3 |
| Magnesium | 1.94 | 1.6–2.6 |
| Calcium | 7.7 | 8.6–10 |
| Test . | Result . | Normal range . |
|---|---|---|
| ALT | 12 | 0–41 |
| S. CREATININE | 2.18 | 0.7–1.2 |
| BUN | 12 | 6–20 |
| S. amylase | 55 | 28–100 |
| S. Sodium | 133 | 135–145 |
| S. Potassium | 4.4 | 3.5–5.3 |
| Magnesium | 1.94 | 1.6–2.6 |
| Calcium | 7.7 | 8.6–10 |
| Test . | Result . | Normal range . |
|---|---|---|
| ALT | 12 | 0–41 |
| S. CREATININE | 2.18 | 0.7–1.2 |
| BUN | 12 | 6–20 |
| S. amylase | 55 | 28–100 |
| S. Sodium | 133 | 135–145 |
| S. Potassium | 4.4 | 3.5–5.3 |
| Magnesium | 1.94 | 1.6–2.6 |
| Calcium | 7.7 | 8.6–10 |
| Test . | Result . | Normal range . |
|---|---|---|
| ALT | 12 | 0–41 |
| S. CREATININE | 2.18 | 0.7–1.2 |
| BUN | 12 | 6–20 |
| S. amylase | 55 | 28–100 |
| S. Sodium | 133 | 135–145 |
| S. Potassium | 4.4 | 3.5–5.3 |
| Magnesium | 1.94 | 1.6–2.6 |
| Calcium | 7.7 | 8.6–10 |
| Test . | Result . | Reference . |
|---|---|---|
| Appearance | Turbid | Clear |
| Color | Bloody | Transparent |
| Sugar | <5 | |
| WBCs | 41 000 | 0–6 |
| RBCs | 500 000 | |
| Culture | E. coli | |
| Cytology | Negative |
| Test . | Result . | Reference . |
|---|---|---|
| Appearance | Turbid | Clear |
| Color | Bloody | Transparent |
| Sugar | <5 | |
| WBCs | 41 000 | 0–6 |
| RBCs | 500 000 | |
| Culture | E. coli | |
| Cytology | Negative |
| Test . | Result . | Reference . |
|---|---|---|
| Appearance | Turbid | Clear |
| Color | Bloody | Transparent |
| Sugar | <5 | |
| WBCs | 41 000 | 0–6 |
| RBCs | 500 000 | |
| Culture | E. coli | |
| Cytology | Negative |
| Test . | Result . | Reference . |
|---|---|---|
| Appearance | Turbid | Clear |
| Color | Bloody | Transparent |
| Sugar | <5 | |
| WBCs | 41 000 | 0–6 |
| RBCs | 500 000 | |
| Culture | E. coli | |
| Cytology | Negative |
| Test . | Result . | Reference . |
|---|---|---|
| Color (urine) | Yellow | (−) |
| Cast | Granular, moderate | (−) |
| Appearance | Clear | (−) |
| Specific gravity | 1.025 | 1.003–1.029 |
| PH urine | Acidic | 4.5–7.8 |
| Protein | Trace | (−) |
| Blood | Rare | (−) |
| WBCs | 6–8 | 0–5 |
| RBCs | 5–7 | 0–5 |
| Epithelial cells | Few | 0–10 |
| Mucus | Large | (−) |
| Bacteria | Nil | (−) |
| Test . | Result . | Reference . |
|---|---|---|
| Color (urine) | Yellow | (−) |
| Cast | Granular, moderate | (−) |
| Appearance | Clear | (−) |
| Specific gravity | 1.025 | 1.003–1.029 |
| PH urine | Acidic | 4.5–7.8 |
| Protein | Trace | (−) |
| Blood | Rare | (−) |
| WBCs | 6–8 | 0–5 |
| RBCs | 5–7 | 0–5 |
| Epithelial cells | Few | 0–10 |
| Mucus | Large | (−) |
| Bacteria | Nil | (−) |
| Test . | Result . | Reference . |
|---|---|---|
| Color (urine) | Yellow | (−) |
| Cast | Granular, moderate | (−) |
| Appearance | Clear | (−) |
| Specific gravity | 1.025 | 1.003–1.029 |
| PH urine | Acidic | 4.5–7.8 |
| Protein | Trace | (−) |
| Blood | Rare | (−) |
| WBCs | 6–8 | 0–5 |
| RBCs | 5–7 | 0–5 |
| Epithelial cells | Few | 0–10 |
| Mucus | Large | (−) |
| Bacteria | Nil | (−) |
| Test . | Result . | Reference . |
|---|---|---|
| Color (urine) | Yellow | (−) |
| Cast | Granular, moderate | (−) |
| Appearance | Clear | (−) |
| Specific gravity | 1.025 | 1.003–1.029 |
| PH urine | Acidic | 4.5–7.8 |
| Protein | Trace | (−) |
| Blood | Rare | (−) |
| WBCs | 6–8 | 0–5 |
| RBCs | 5–7 | 0–5 |
| Epithelial cells | Few | 0–10 |
| Mucus | Large | (−) |
| Bacteria | Nil | (−) |
A computed tomography scan without contrast (due to elevated s.creatinine of 2.18) revealed a moderate to severe amount of free fluid in the abdominal and pelvic cavities. The appendix was perforated. The juojenal bowel loops and the rectum showed circumferential wall thickening mostly due to inflammatory process (Figs 1 and 2).
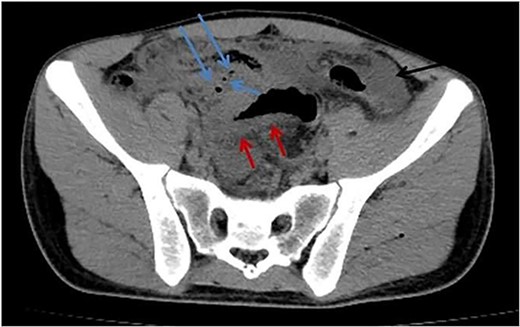
Axial abdomen CT scan without contrast shows pneumoperitoneum (blue arrows), free fluid (black arrow), and sigmoid wall thickening (red arrow).
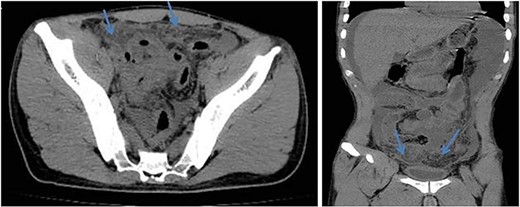
Axial (left) and coronal (right) views of abdomen CT scan without contrast show dirty fat planes closely related to the urinary bladder walls (mass formation).
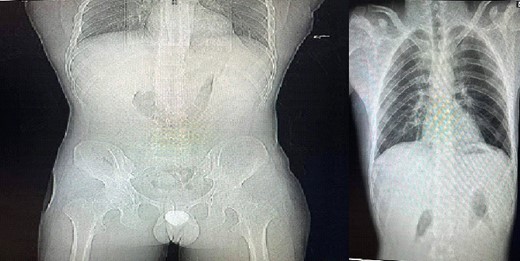
Chest X-ray and standing abdominal X-ray revealed pneumoperitoneum (Fig. 3).
Abdominal exploration revealed an appendicular mass with perforated appendix surrounded by omentum and attached to the urinary bladder and sigmoid colon. About 1800 cc of turbid fluid were suctioned, followed by washing with warm saline. Intact urinary bladder insured by injection of methylene blue with no oozing to abdominal cavity. Appropriate drains were inserted. The patient improved clinically and his labs normalized. The postoperative course was uneventful with no postoperative complications, then the patient discharged home well.
Intraoperative findings
The appendix was dilated, with its distal end connected to the urinary bladder with mass formation and friable tissue (Fig. 4).
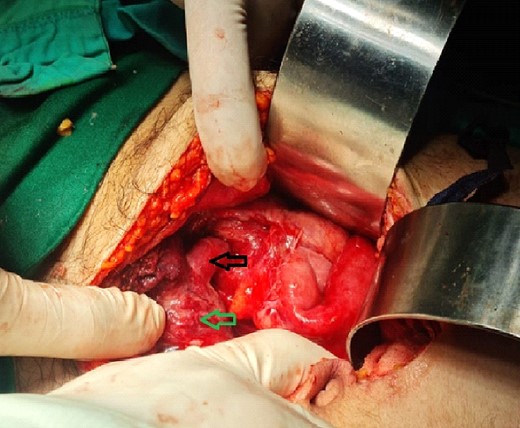
Intraoperative findings; black arrow: appendix, green arrow: urinary bladder.
Discussion
Acute appendicitis is rarely caused by abdominal trauma. However, it is difficult to establish the direct association. A greater rate of appendicitis in pediatric patients following acute abdominal injuries is reported [1]. Traumatic appendicitis can be defined by: (1) absence of prior history of abdominal attacks; (2) severe indirect or direct abdominal wall trauma; (3) early beginning of symptoms following the trauma; and (4) progressive symptoms necessitating treatment and appendicitis diagnosis [2].
Information on the pathophysiology of traumatic appendicitis is scarce. Direct trauma can result in blockage and acute appendicitis via edema and inflammation of the appendicular lymphoid tissue. When there is indirect trauma, a rise in intra-abdominal pressure can lead to a rise in intracecal pressure, which can quickly develop appendicitis and appendiceal distension. There have also been reports of direct trauma to the mesoappendix [3]. One patient developed traumatic appendicitis after experiencing perineal trauma [4]. These mechanisms remain theoretical even though they could be combined or isolated.
Traumatic appendicitis typically presents similarly to appendicitis that is not caused by trauma [5].
The urologic literature provides a thorough description of microscopic hematuria as an accidental finding in patients with acute appendicitis [6]. The majority of these instances had a clinically evident diagnosis of appendicitis, with hematuria being caused by the inflamed appendix next to the ureter or bladder. Occasionally, though, a patient may appear primarily with urologic symptoms, making the diagnosis of appendicitis challenging. With our patient, this was the situation.
Computed tomography is a useful and non-invasive technique for determining the nature and extent of an indeterminate lower abdominal mass [7].
The unexpected complication of acute appendicitis with an appendicular inflammatory mass extending to the urinary bladder in our adult male patient following blunt abdominal trauma merits a comprehensive discussion. This rare scenario prompts a closer examination of the intricate relationship between trauma and appendicitis, emphasizing the need for increased awareness among healthcare providers.
The right lower quadrant is the usual location for an appendiceal abscess, also known as phlegmon. However, because the appendix can vary greatly in size and location, an abscess can also spread into the pelvis and affect the bladder. A perforated cecal or appendiceal carcinoma, pelvic inflammatory disease, Crohn’s disease, and cecal diverticulitis are a few examples of inflammatory conditions that can cause an abscess and resemble appendicitis [8]. The presence of a single, dense calcification located in the center of the infiltrative mass raises serious doubts about the identity of the mass being an appendicolith and may be pathognomonic for appendicitis [9].
Conclusion
In conclusion, the presented case underscores the significance of a thorough evaluation in the setting of postblunt abdominal trauma. Clinicians must be attuned to the potential coexistence of unusual complications, such as acute appendicitis, and consider the nuances of management when intricate structures like the urinary bladder are involved. This case report serves as a valuable contribution to the evolving landscape of trauma-related complications, emphasizing the need for ongoing research and collaborative learning within the medical community.
Conflict of interest statement
None declared.
Funding
None declared.



