-
PDF
- Split View
-
Views
-
Cite
Cite
Darwin R Ramos, Antonio S Robalino, Daniel L Mogrovejo, Doménica A Suárez, Aitana E Ross Proaño, Diana E Parrales, Gabriel A Molina, An uninvited guest, Ascaris in the bile duct causing cholangitis successfully treated with surgery, Journal of Surgical Case Reports, Volume 2024, Issue 4, April 2024, rjae264, https://doi.org/10.1093/jscr/rjae264
Close - Share Icon Share
Abstract
Parasitic infections continue to be a burden for developing countries—the lack of hygiene measures and clean water results in dangerous scenarios that can lead to challenging problems. Most Ascaris lumbricoides infections are usually mild; nonetheless, in rare cases in endemic regions, they can migrate to the bile duct and cause severe complications requiring surgery. We present the case of a 43-year-old woman who had severe cholangitis due to A. lumbricoides. The worm migrated from the bowel and obstructed the bile duct; after surgery, the patient fully recovered.
Introduction
Ascariasis, caused by Ascaris lumbricoides, is the most common gastrointestinal parasitic infection worldwide; it especially thrives in countries where sanitation practices are poor [1, 2]. This disease is usually mild; however, on rare occasions, it can invade the biliary tract, leading to various complications, including cholecystitis, pyogenic cholangitis, and liver abscesses [1–3].
We present the case of a young woman with cholangitis due to A. lumbricoides; after surgery, the worm was removed, and the patient recovered successfully.
Case report
The patient is a 43-year-old woman who lives in a remote area of the city with little access to clean water. She arrived at the emergency department with upper abdominal pain. She had been suffering from this pain for more than a year; nonetheless, in the last 6 months, the pain had become more intense and was accompanied by recurrent episodes of abdominal distension, nausea, vomiting, anorexia, and intermittent diarrhea.
Clinical examination revealed a jaundiced, malnourished, and tachycardic patient. In addition, intense pain and tenderness were detected in the right upper abdomen. Pale stools and dark urine were also observed.
Initial blood workup revealed leukocytosis (16 400/mm3) with neutrophilia (89.5%); her pancreatic enzymes were normal; lipase levels were registered at 75.7 U/l and amylase at 28 U/l. Bilirubin levels were elevated (18 mg/dl), and gamma-glutamyl transferase was at 863 U/l. Blood gas analysis reported a pH of 7.34, with lactic acid at 1.61. The PaO2/FiO2 ratio was 337, and creatinine was measured at 1.18 mg/dl.
With these findings, it was necessary to perform an ultrasound. It revealed a distended gallbladder with sludge and a dilated common bile duct. A straight, non-shadowing echoic cord-like structure without a central hypoechoic tube was noticed within it (Figs 1a and 2b).

(A) Echography shows the bile duct dilated with the Ascaris inside it; (B) echography is a straight, non-shadowing echoic cord-like structure in the bile duct.
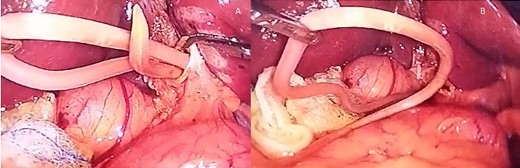
(A) The Ascaris is seen inside the bile duct; (B) the Ascaris is completely removed from the bile duct, choledochotomy is seen as well.
Cholangitis and bile duct obstruction due to A. lumbricoides were suspected, and due to this, broad-spectrum antibiotics were initiated. An endoscopic retrograde cholangiopancreatography was planned; nonetheless, that procedure was unavailable at the time in our hospital; therefore, surgery was decided since the patient’s condition was rapidly deteriorating.
At laparoscopy, multiple adhesions from the omentum to the gallbladder were found. The adhesions were released, and after the bile duct was exposed, a 1.5 cm choledochotomy was done.
Purulent bile was drained, and a 12 × 1.5 cm A. lumbricoides was found in the bile duct, causing complete obstruction. The roundworm was removed, and a cholangiogram was done afterward, ensuring that the bile duct was clear (Fig. 2a and b).
A choledocoplasty with an absorbable suture was done in a one-layer fashion with 2-0 PDS (Ethicon, Johnson & Johnson Intl.) The gallbladder was removed, a drain was placed, and the rest of the procedure was completed without complications.
The patient’s postoperative course was uneventful. She fully recovered after surgery and broad-spectrum antibiotics and anthelmintics. The drain was removed on the fifth postoperative day, and afterward, she was discharged without complications. On follow-ups, the patient is doing well; she was advised to improve her and her family’s dietary and hygienic traditions, to boil water, and to wash her hands.
Discussion
A. lumbricoides is an intestinal nematode which was first described by Carl Linnaeus in 1758 and is the causative agent of the human disease ascariasis, which affects more than 1.2 billion people every year [1, 2]. The epidemiology of Ascaris infection has changed in the past decade thanks to improved sanitation and oral anthelminthic agents. Nowadays, it mainly affects developing countries with poor hygiene practices, like the Indian subcontinent, China, the African continent, and Latin America [1]. In countries like Ecuador, hygiene practices are worrisome (inadequate hand washing, poor drinking water, and unhygienic defecation practices), leading to more infections [3]. In our case, the patient lived in a marginal area with poor access to water and had poor hygiene habits, which led to her severe infection.
When an infected egg is swallowed, it travels to the bowel, and the larvae hatch in the small intestine; then, it migrates to the colon, infiltrating its mucosa and reaching the liver [1, 4]. Once there, it advances to the lungs, crossing the alveolar space and moving to the pharynx [1, 3, 4]. Once there, they are swallowed again and returned to the bowel, where they can reach sexual maturity [4]. Although the majority of infections are asymptomatic, up to 15% of infected may present with varied gastrointestinal (malnutrition, abdominal pain, bloating, nausea, vomiting, anorexia, intermittent diarrhea), pulmonary (wheezing, dyspnea, cough, hemoptysis, and fever) and neurological symptoms [5, 6].
In rare cases of severe infection in which there is a large population of worms in the bowel, the adult worms can migrate to the biliary and pancreatic systems, causing obstruction and inflammation. This leads to severe complications like cholecystitis, cholangitis, liver abscess, and pancreatitis [1]. The continuous pressure on the biliary tract can even cause bile duct perforation with perforation and peritonitis [1, 5]. In our case, the worm migrated to the bile duct, causing cholangitis.
Treatment with benzimidazole has a cure rate of 96.6% and an egg reduction rate of 99.9% [1, 7]. Still, reinfection can happen if patients continue to engage in poor health practices [1–3]. Patients with biliary ascariasis will not respond to standard anthelminthic drugs because their biliary excretion is low; therefore, the worms must first be removed from the biliary tract to eliminate the infection [8, 9].
Endoscopic intervention has become the treatment of choice, and worms visible at the ampulla may be removed endoscopically [1, 9]. Sphincterotomy should be avoided because it can facilitate future recurrence if worm reinfestation occurs [9, 10]. Surgery is reserved for patients who fail to respond to medical management or show evidence of complications [1, 2, 9].
In our case, since the patient’s condition was deteriorating and endoscopic therapy was not available at the time, surgery was decided. We were able to remove the obstruction and improve the patient’s condition. Postoperative follow-up was vital in our case since the patient had to change not only her habits but also those of her family to avoid further reinfections and reduce complications.
Conclusion
Ascariasis is the most common helminthic infection worldwide, and it can be a severe burden for developing countries that lack basic sanitation routines. In these endemic regions, on rare occasions, the worms can migrate to the biliary tract and cause severe complications. It is up to the medical team to face these challenges promptly using medical, endoscopic, and surgical therapies to treat these rare scenarios.
In developing countries, the medical team must go beyond only treating patients. To control this severe problem and minimize reinfections, we must increase awareness of hygiene and safe sanitary practices among all our patients.
Conflict of interest statement
None declared.
Funding
None declared.



