-
PDF
- Split View
-
Views
-
Cite
Cite
Andrej Nikolovski, Dajana Cako, Ivan Argirov, Nimetula Limani, Cemal Ulusoy, Chevrel’s procedure for midline incisional hernia repair—not to be abandoned or forgotten, Journal of Surgical Case Reports, Volume 2024, Issue 10, October 2024, rjae643, https://doi.org/10.1093/jscr/rjae643
Close - Share Icon Share
Abstract
The Chevrel technique is a well-established procedure for open repair of midline incisional hernia. This retrospective single-center case series aims to present the outcome of patients with midline incisional hernia treated with a modified Chevrel technique. The modification itself comprehended the use of a single-layer continuous suture for the inverted anterior rectus abdominis muscle sheet for the creation of the “new linea alba” without overlapping. Between January 2017 and December 2023, 40 patients were operated. The overall postoperative morbidity rate was 65%. Hernia recurrence occurred in three patients (7.5%). When the basic principles of the Chevrel technique are respected and conducted, this leads to satisfactory results. The postoperative outcome of this case series showed rates of complications and recurrences in concordance with the already published literature. Therefore, this technique should always be considered for the open approach for midline incisional hernia repair.
Introduction
Both, emergency and elective open abdominal, gynecology, vascular, and urology procedures (including patients with abdominal trauma) often require access via the midline laparotomy. Subsequently, the risk of midline incisional hernia (MIH) occurrence in such patients is a reality. The incidence of incisional hernia after midline laparotomy is 11% while in emergency settings this rate is reported to be even higher (18.1%) [1, 2].
When open MIH repair is considered, different techniques with or without a synthetic mesh implant are available such as the component separation technique described by Ramirez et al. the Rives repair, and the Chevrel repair [3–5].
The recommendations on the treatment of midline incisional hernias were recently published by the European Hernia Society (EHS). The group focused exclusively on this most common type of incisional hernia. According to EHS, a technique with retromuscular mesh placement is strongly recommended for patients with MIH. However, despite the strong recommendation, the level of evidence has very low certainty [6].
The onlay method is described to be much simpler to learn and perform and, at the same time, results in a low recurrence rate of ~5% of cases [7, 8]. Chevrel procedure has certain technical advantages over the rest of the procedures described for MIH repair: it can be used both, in high and low midline incisional hernias, the opening of the hernia sac during the procedure is not necessary, a re-creation of “new linea alba” by re-approximation of the rectus abdominis muscles (anterior abdominal wall anatomy restoration) is a part of the procedure, mesh infection presence does not require its extraction in most cases and it is easier to treat, the risk for intraperitoneal mesh migration and erosion with consecutive enteric fistula formation is minimal [9, 10]. This case series aimed to investigate the outcomes of the treatment of midline incisional hernia by the use of the Chevrel technique.
Materials and methods
Study design and patient selection
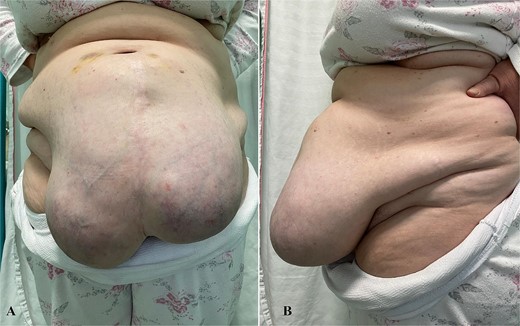
This retrospective observational case series included patients treated for midline incisional hernias between January 2017 and December 2023 with the Chevrel technique. All the patients were diagnosed with physical examination (Fig. 1) and abdominal computerized tomography (CT) scans (Fig. 2). The midline incisional hernia was classified according to the EHS classification [11].
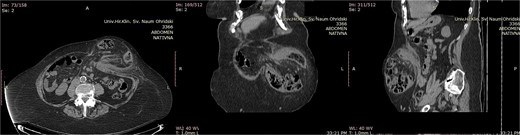
Abdominal computerized tomography scan of a patient with M3W2 incarcerated incisional hernia. The incarcerated loop of the transverse colon is visible in the hernia sac (A-axial scan, B-coronal scan, C-sagittal scan).
Preparation for surgery
To all patients, 2 gm of cephalosporin (third generation) were given intravenously 60 minutes before skin incision and continued in the postoperative period for 3 days. Patients were operated in general endotracheal anesthesia. Three surgeons from the department performed all the procedures. Antithrombotic prophylaxis with low molecular weight heparin was conducted in dosage according to individual patient weight.
Operative method
Excision of the previous scar was selectively performed depending on the skin quality. In basic, the described Chevrel technique [9] was used while keeping in mind the principles of the procedure (creation of new linea alba and approximation of the rectus abdominis muscles). The modification employed when suturing the inverted anterior rectus abdominis sheets was that only a single layer with continuous polypropylene 0 suture was used, without overlapping. A macroporous polypropylene mesh was used. The mesh was positioned and fixed with 0 single polypropylene sutures. The size of the used mesh was determined intraoperatively by keeping the principles for covering the incised anterior rectus sheets (Fig. 3). Two subcutaneous active-suction drains (Redon-16 Ch.) were placed over the mesh. Subcutaneous fat was closed with a 2-0 continuous monofilament absorbable suture. A 3-0 single monofilament suture was employed for skin closure (Video s1). For some patients, a simultaneous procedure was performed.
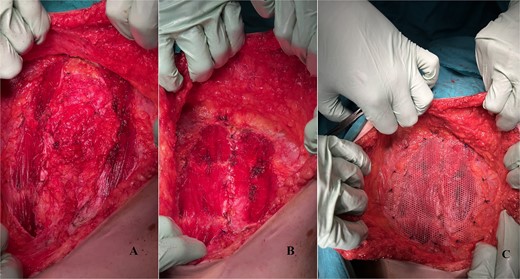
Intraoperative photos. (A) Incised anterior rectus sheet on both sides. (B) The overlapped rectus sheet sutured, “new linea alba” was created and the rectus abdomins muscles approximated. (C) Polypropylene mesh implanted and fixed onlay.
Postoperative measures
All patients wore an abdominal binder in the postoperative period for 30 days. Oral liquid taking and feeding started on postoperative Day 1 in parallel with patient mobilization. Drain removal was decided when <50 ml of serosal fluid per 24 hours was collected, followed by discharge from the hospital.
Follow-up
Surgical Site Event and other complications were noted within the first 30 days after surgery. Patients were followed in the outpatient ward in the first 6 months after surgery and later by telephone interview. In cases of complaints, they were invited for physical examination. Abdominal CT scans were used to confirm recurrences.
Results
A total number of 40 patients with a mean age of 60.7 years were treated, 17 of them male, and the rest female. Eleven of them were reported to be active cigarette smokers. Comorbidities (hypertension, deep vein thrombosis, and diabetes mellitus) were reported by 33 patients. The majority of the patients presented with an ASA score of 3. Elective surgery was performed on 32 patients, while the rest 8 were treated due to emergency presentation (hernia incarceration). In one patient from the emergency group, a partial bowel resection of the transverse colon with primary anastomosis was performed. The most common presentation of the incisional hernia was classification M4 W2 (Table 1).
| Variable . | N (%) . |
|---|---|
| Age mean [range] | 60.7 [43–82] |
| Gender | |
| Male | 17 (42.5) |
| Female | 23 (57.5) |
| Active cigarette smoker | |
| Yes | 11 |
| No | 29 |
| Comorbidity | |
| Deep vein thrombosis | 4 |
| Hypertension | 26 |
| Diabetes mellitus | 3 |
| Previous midline laparotomy procedure | |
| Cesarean section | 7 |
| Peptic ulcer disease complication | 6 |
| Colorectal cancer procedure | 4 |
| Transabdominal vascular procedure | 5 |
| Open hiatal hernia repair | 1 |
| Appendectomy | 2 |
| Open gynecologic procedure | 9 |
| Complicated colonic diverticulitis | 1 |
| Intraabdominal injury | 1 |
| Adhesive ileus | 3 |
| Excision of urachal cyst | 1 |
| ASA score | |
| 2 | 11 |
| 3 | 23 |
| 4 | 6 |
| Hernia presentation | |
| Elective | 32 (80) |
| Emergency | 8 (20) |
| EHS classification | |
| M2 W1 | 1 |
| M2 W2 | 7 |
| M3 W1 | 2 |
| M3 W2 | 12 |
| M3 W3 | 1 |
| M4 W1 | 1 |
| M4 W2 | 15 |
| M4 W3 | 1 |
| Variable . | N (%) . |
|---|---|
| Age mean [range] | 60.7 [43–82] |
| Gender | |
| Male | 17 (42.5) |
| Female | 23 (57.5) |
| Active cigarette smoker | |
| Yes | 11 |
| No | 29 |
| Comorbidity | |
| Deep vein thrombosis | 4 |
| Hypertension | 26 |
| Diabetes mellitus | 3 |
| Previous midline laparotomy procedure | |
| Cesarean section | 7 |
| Peptic ulcer disease complication | 6 |
| Colorectal cancer procedure | 4 |
| Transabdominal vascular procedure | 5 |
| Open hiatal hernia repair | 1 |
| Appendectomy | 2 |
| Open gynecologic procedure | 9 |
| Complicated colonic diverticulitis | 1 |
| Intraabdominal injury | 1 |
| Adhesive ileus | 3 |
| Excision of urachal cyst | 1 |
| ASA score | |
| 2 | 11 |
| 3 | 23 |
| 4 | 6 |
| Hernia presentation | |
| Elective | 32 (80) |
| Emergency | 8 (20) |
| EHS classification | |
| M2 W1 | 1 |
| M2 W2 | 7 |
| M3 W1 | 2 |
| M3 W2 | 12 |
| M3 W3 | 1 |
| M4 W1 | 1 |
| M4 W2 | 15 |
| M4 W3 | 1 |
| Variable . | N (%) . |
|---|---|
| Age mean [range] | 60.7 [43–82] |
| Gender | |
| Male | 17 (42.5) |
| Female | 23 (57.5) |
| Active cigarette smoker | |
| Yes | 11 |
| No | 29 |
| Comorbidity | |
| Deep vein thrombosis | 4 |
| Hypertension | 26 |
| Diabetes mellitus | 3 |
| Previous midline laparotomy procedure | |
| Cesarean section | 7 |
| Peptic ulcer disease complication | 6 |
| Colorectal cancer procedure | 4 |
| Transabdominal vascular procedure | 5 |
| Open hiatal hernia repair | 1 |
| Appendectomy | 2 |
| Open gynecologic procedure | 9 |
| Complicated colonic diverticulitis | 1 |
| Intraabdominal injury | 1 |
| Adhesive ileus | 3 |
| Excision of urachal cyst | 1 |
| ASA score | |
| 2 | 11 |
| 3 | 23 |
| 4 | 6 |
| Hernia presentation | |
| Elective | 32 (80) |
| Emergency | 8 (20) |
| EHS classification | |
| M2 W1 | 1 |
| M2 W2 | 7 |
| M3 W1 | 2 |
| M3 W2 | 12 |
| M3 W3 | 1 |
| M4 W1 | 1 |
| M4 W2 | 15 |
| M4 W3 | 1 |
| Variable . | N (%) . |
|---|---|
| Age mean [range] | 60.7 [43–82] |
| Gender | |
| Male | 17 (42.5) |
| Female | 23 (57.5) |
| Active cigarette smoker | |
| Yes | 11 |
| No | 29 |
| Comorbidity | |
| Deep vein thrombosis | 4 |
| Hypertension | 26 |
| Diabetes mellitus | 3 |
| Previous midline laparotomy procedure | |
| Cesarean section | 7 |
| Peptic ulcer disease complication | 6 |
| Colorectal cancer procedure | 4 |
| Transabdominal vascular procedure | 5 |
| Open hiatal hernia repair | 1 |
| Appendectomy | 2 |
| Open gynecologic procedure | 9 |
| Complicated colonic diverticulitis | 1 |
| Intraabdominal injury | 1 |
| Adhesive ileus | 3 |
| Excision of urachal cyst | 1 |
| ASA score | |
| 2 | 11 |
| 3 | 23 |
| 4 | 6 |
| Hernia presentation | |
| Elective | 32 (80) |
| Emergency | 8 (20) |
| EHS classification | |
| M2 W1 | 1 |
| M2 W2 | 7 |
| M3 W1 | 2 |
| M3 W2 | 12 |
| M3 W3 | 1 |
| M4 W1 | 1 |
| M4 W2 | 15 |
| M4 W3 | 1 |
In three patients, a simultaneous procedure was performed (dermolipectomy, bilateral adnexectomy, and partial transverse colon resection with primary anastomosis).
The mean operative time was 144 minutes. No in-hospital mortality was noted. The overall postoperative morbidity rate was 65%. Two patients were admitted for intensive unit care in the postoperative period.
In one female patient (M4 W3 hernia classification) with a previous medical history of deep vein thrombosis, a pulmonary insufficiency developed (mild oxygen saturation drop) on postoperative Day 2 and was treated in the intensive care unit with non-invasive measures with 6 L of 100% oxygen per minute and respiratory exercises. A contrast-enhanced pulmonary CT scan excluded pulmonary embolism.
In one female patient, a deep vein thrombosis of the right lower extremity was detected and was treated conservatively. Additionally, a wound dehiscence occurred and was treated with a negative wound pressure device. In three patients, significant postoperative anemia occurred due to retroperitoneal hematoma and was treated with units of blood.
A significant drop in hemoglobin level (<85 g/L) due to retroperitoneal hematoma presence was noted in four patients and units of blood were given as a treatment.
The overall operative wound complication rate was 57.5%. Wound seroma was the most common surgical site event (17.5 %), followed by superficial wound infection (15%), wound dehiscence (10%), wound hematoma (7.5%), and partial skin necrosis (7.5%). A mesh infection as a late complication occurred in one patient. The median length of hospital stay was 8.4 days (Table 2).
| Variable . | N (%) . |
|---|---|
| Mean operative time [range] | 144 minutes [67–280] |
| Respiratory insufficiency | 1 |
| Intensive care admission | 2 |
| Lower extremity deep vein thrombosis | 1 |
| Postoperative hemoglobin level below 85 g/L (retroperitoneal hematoma) | 3 |
| Postoperative blood units given per patient | |
| 1 unit | 1 |
| 2 units | 1 |
| 7 units | 1 |
| Surgical Site Event | |
| Wound seroma | 7 (17.5) |
| Wound infection (superficial) | 6 (15) |
| Wound hematoma | 3 (7.5) |
| Wound dehiscence | 4 (10) |
| Partial skin necrosis | 3 (7.5) |
| Mesh infection | 1 (2.5) |
| Median length of hospital stay in days [range] | 8.4 [4–117] |
| Hernia recurrence | 3 (7.5) |
| Variable . | N (%) . |
|---|---|
| Mean operative time [range] | 144 minutes [67–280] |
| Respiratory insufficiency | 1 |
| Intensive care admission | 2 |
| Lower extremity deep vein thrombosis | 1 |
| Postoperative hemoglobin level below 85 g/L (retroperitoneal hematoma) | 3 |
| Postoperative blood units given per patient | |
| 1 unit | 1 |
| 2 units | 1 |
| 7 units | 1 |
| Surgical Site Event | |
| Wound seroma | 7 (17.5) |
| Wound infection (superficial) | 6 (15) |
| Wound hematoma | 3 (7.5) |
| Wound dehiscence | 4 (10) |
| Partial skin necrosis | 3 (7.5) |
| Mesh infection | 1 (2.5) |
| Median length of hospital stay in days [range] | 8.4 [4–117] |
| Hernia recurrence | 3 (7.5) |
| Variable . | N (%) . |
|---|---|
| Mean operative time [range] | 144 minutes [67–280] |
| Respiratory insufficiency | 1 |
| Intensive care admission | 2 |
| Lower extremity deep vein thrombosis | 1 |
| Postoperative hemoglobin level below 85 g/L (retroperitoneal hematoma) | 3 |
| Postoperative blood units given per patient | |
| 1 unit | 1 |
| 2 units | 1 |
| 7 units | 1 |
| Surgical Site Event | |
| Wound seroma | 7 (17.5) |
| Wound infection (superficial) | 6 (15) |
| Wound hematoma | 3 (7.5) |
| Wound dehiscence | 4 (10) |
| Partial skin necrosis | 3 (7.5) |
| Mesh infection | 1 (2.5) |
| Median length of hospital stay in days [range] | 8.4 [4–117] |
| Hernia recurrence | 3 (7.5) |
| Variable . | N (%) . |
|---|---|
| Mean operative time [range] | 144 minutes [67–280] |
| Respiratory insufficiency | 1 |
| Intensive care admission | 2 |
| Lower extremity deep vein thrombosis | 1 |
| Postoperative hemoglobin level below 85 g/L (retroperitoneal hematoma) | 3 |
| Postoperative blood units given per patient | |
| 1 unit | 1 |
| 2 units | 1 |
| 7 units | 1 |
| Surgical Site Event | |
| Wound seroma | 7 (17.5) |
| Wound infection (superficial) | 6 (15) |
| Wound hematoma | 3 (7.5) |
| Wound dehiscence | 4 (10) |
| Partial skin necrosis | 3 (7.5) |
| Mesh infection | 1 (2.5) |
| Median length of hospital stay in days [range] | 8.4 [4–117] |
| Hernia recurrence | 3 (7.5) |
The follow-up period ranged between 6 and 84 months. A total number of 37 (92.5%) patients were followed, and the rest were lost. During the follow-up period, three patients (7.5%) presented with clinical hernia recurrence confirmed by abdominal CT scans.
Discussion
Chevrel and Browse independently of one other introduced similar repair methods for MIH by the use of reflected flaps of the anterior rectus sheath (“overcoat” plasty) with onlay mesh reinforcement [5, 12]. The essence of this technique lies in two principles: new linea alba creation and position restoration of the rectus abdominis muscles [13]. In the cadaveric study of Rath and Chevrel, the importance of the re-creation of linea alba in MIH repair with the anterior rectus sheath comes from its strength. Namely, they concluded that the anterior supra-arcuate rectus sheath was the strongest part of the abdominal wall, and its use is justifiable [14, 15].
Schug-Pass et al. point out the importance of creating new linea alba which leads to anatomical reconstruction and achievement of the “dynamic repair of the abdominal wall”. The authors conclude that a midline reconstruction is mandatory to facilitate a successful midline incisional hernia repair with a relatively tension-free closure [16].
When it comes to the limitations of certain techniques dictated by the midline hernia defect size, the Rives-Stoppa procedure was recommended for defects with widths up to 8 cm. Its restrictions come to the fore when retro rectus space is atrophied or obliterated by fibrosis or by previously implanted mesh [17].
In cases of giant midline incisional hernia existence (W3), with a diameter >10 cm, there is no consensus on which of the techniques should be used. In the national survey of Passot et al. none of the procedures gained major support from the responders. Still, the authors concluded that besides the hernia defect size, the pre-operative respiratory and cutaneous preparation is equally important in the preoperative patient assessment [18].
In the systematic review of Deerenberg et al. [19], with 55 articles and 3945 patients with incisional hernia surgery included, a sublay position of the mesh for giant incisional hernia repair is recommended [19]. Haskins et al. [20] recommend Chevrel’s technique to be selective, including non-obese patients without significant comorbidities and moderate hernia defects.
In this series, a patient's maximal width of the hernia defect was 126 mm (W3). In our opinion, treating giant midline incisional hernias with defect size >15 cm by Chevrel’s technique might be technically unfeasible. Our secondary concern is the possibility of postoperative abdominal compartment syndrome development. The components separation technique could overcome these limitations.
According to Alemanno et al. [21], Chevrel’s procedure is safe and easy to perform and results in satisfactory immediate and late results. In our opinion, the vast majority of patients with midline incisional hernia could be managed with Chevrel’s technique and it should not be abandoned or forgotten at all.
Another advantage of the on-lay mesh position is the lowest risk for enterocutaneous fistula formation in comparison to the intraperitoneal, preperitoneal, and retromuscular mesh positions. At the same time, the on-lay position is favorable when mesh infection occurs, regardless of the type of infection treatment (conservative, vacuum-assisted closure, or mesh removal) [22].
The reported mean postoperative complication rate after incisional hernia surgery with the onlay technique is 33.5% with a range of 5%–76% [23]. In the series of Chevrel, the overall morbidity rate was 10.5%. He reported seroma occurrence in 6.3% and a superficial wound infection rate of 2.8% [9]. In the prospective randomized controlled trial of Kaafarani et al. [24], seroma was reported in 16.6% out of 145 patients (including the ones in whom a conversion from laparoscopic to open hernia repair was done). Licheri et al. [25] report a rate of 26.5% of early postoperative complications. Seroma was encountered in 11%, skin necrosis in 8%, and superficial wound infection in 5% of the patients. Mommers et al. [26] report a surgical site occurrence rate of 19.4%, seroma incidence of 10.3%, and surgical site infection (SSI) rate of 5.8%. Alemanno et al. [21] report parietal complications in terms of seroma (7.1%), hematoma (4.7%), localized skin necrosis (5.2%), and surgical site infection (6.7%) occurrence. Hodgman and Watson report a rate of surgical site complications of 31% [10]. In this series, the rates of surgical site events were within the previously published ranges.
Controversies exist on whether mesh should be used in the emergency setting taking into consideration possible surgical site and/or mesh infection due to the operative field contamination during the emergency hernia repair. Birolini et al. [27] treated 20 patients with large bowel resection and bowel continuity reestablishment in concomitance with incisional hernia repair by the use of polypropylene mesh positioned over the rectus sheath. A wound infection was reported in one patient (infection rate of 5%). Nieuwenhuizen et al. reported 38 patients with incarcerated/strangulated incisional hernia of whom 19 were treated with mesh repair. In nine of them, bowel resection was performed, and two patients suffered from wound infection (infection rate of 22.2%). In their study, the major factor associated with wound infection was bowel resection [28]. In the series of Emile et al. a total number of 66 patients with incarcerated and strangulated incisional hernia were treated with polypropylene mesh repair positioned onlay. No statistically significant difference was found between the groups with mesh and suture repair. Similarly, the analysis of the incarcerated and strangulated hernia groups resulted in no difference in the SSI rates [29]. In this series, the only patient treated with concomitant partial large bowel resection (clean-contaminated wound classification) with primary anastomosis presented with SSI and wound dehiscence.
Major postoperative complications (abdominal compartment syndrome, deep vein thrombosis, pulmonary complications) and in-hospital mortality following giant incisional hernia repair represent a real threat to the desired outcome [30]. The reported rate of major postoperative complications is 5.8% [26]. The reported range of mortality is 0.4%–10.4% and is associated with the incisional hernia complexity and not with the technique [19, 25].
The overall recurrence rate for onlay incisional hernia repair in the systematic review of Köckerling was 9.9%, with a range of 0% and 32% [23]. Most of the reports show recurrence rates between 0% and 7.3% in a heterogeneous follow-up period between 0 months and 20 years [9, 13, 21, 25, 26, 31, 32]. This series reports a hernia recurrence rate within the published literature ranges.
Conclusion
Chevrel technique modification presented in this series is effective in the treatment of midline incisional hernias. Following the recently published reports, it offers acceptable major and minor postoperative complication rates and hernia recurrence rates. However, in cases with giant midline incisional hernia (defect width >15 cm), an alternative procedure should be contemplated due to the possibility of not gaining an adequate position restoration of the rectus abdominis muscles for primary fascial closure. Still, the Chevrel technique should always be kept in mind when one is considering an open approach for midline incisional hernia repair.
Acknowledgements
Andrej Nikolovski thanks Prof. Dragoslav Mladenović (the one who left us too soon). He taught me a lot about hernia and surgery, in general.
Author contributions
Andrej Nikolovski (Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Writing—original draft, Writing—review & editing), Dajana Cako (Data curation, Formal analysis, Methodology, Writing—review & editing), Nimetula Limani (Data curation, Investigation, Methodology, Writing—review & editing), and Cemal Ulusoy (Conceptualization, Methodology, Supervision, Writing—review & editing).
Conflict of interest statement
The authors declare no conflict of interest
Funding
There is no funding to declare.
Data availability
Data is available upon reasonable request.



