-
PDF
- Split View
-
Views
-
Cite
Cite
Falk Nessenius, Isabel Zucal, Jürgen-Klaus Allmann, Stefan Spreitzer, Regula Marti, Incidental deep soft tissue leiomyoma of the groin – a case report and comprehensive review of literature, Journal of Surgical Case Reports, Volume 2024, Issue 1, January 2024, rjae020, https://doi.org/10.1093/jscr/rjae020
Close - Share Icon Share
Abstract
Leiomyomas are rare, benign tumors arising from smooth muscle cells. Due to the heterogeneous anatomical locations, as well as clinical and radiological findings, early and correct diagnosis is usually tricky. The clinical symptoms depend on the anatomical structure the tumors are compromising by their growth. We present a case of a 53-year-old male patient who suffered from swelling of the right foot and ankle. Initially, arthritis and deep vein thrombosis were ruled out. As the swelling progressed to the entire leg, CT scan was performed showing a tumor compressing the right femoral vein. However, a magnetic resonance imaging (MRI) and a biopsy did not show any conclusive findings. Tumor excision was planned and immunohistochemical staining confirmed leiomyoma. The authors conclude that unspecific, progressive symptoms should prompt further investigation and whenever planning a biopsy, a possible malignant finding should be considered and excision of the biopsy canal together with the tumor must be assured.
Introduction
Deep soft tissue leiomyomas (DSTL) are benign and very rare tumors, representing 4.4% of all benign soft tissue neoplasms [1–3]. They derive from smooth muscle cells and are classified into cutaneous, vascular and deep soft tissue leiomyomas [2, 4]. DSTL are further divided into vascular and non-vascular [2]. According to Weiss [5], there is a clinicopathological distinction between tumors with no sex prevalence arising from deep somatic soft tissue and tumors occurring particularly in women in the pelvic retroperitoneum. In contrast to the more common leiomyoma of the uterus or the retroperitoneum [6, 7], DSTL of the lower extremity are extremely rare findings and in literature, mainly case reports exist [4].
They usually appear in adults between the fourth and fifth decade of age [8]. Depending on the anatomical location and the anatomical structures their growth is compressing, the clinical presentation varies and very often, several diagnostic examinations are required before identifying the tumor. Once found and excised, histological confirmation of a soft tissue leiomyoma is not easy. In fact, not only the clinical location and presentation are heterogeneous, but also the genetic changes have been described to be heterogeneous in DSTL [6]. Therefore, the pathway from the initial clinical presentation to the final correct diagnosis may include several detours defined by misleading symptoms and clinical findings. Consequently, multiple steps in the diagnostic latter may be required.
Case report
A 53-year-old, otherwise healthy patient presented with a swelling of the right foot and ankle since 4 months. The patient denied previous trauma, B-symptoms and intermittent claudication. Clinical examination showed edema of the aforementioned regions, and no signs of infection. Deep vein thrombosis was ruled out by ultrasound. X-rays and serological examinations showed no signs of arthritis. A CT-scan was performed 1 month after initial presentation due to progressive swelling of the leg and showed a change in diameter of the common femoral vein due to compression of a hyperechogenic structure in the groin. These findings were confirmed by duplex sonography, showing a structure with a diameter of 3 cm compressing the femoral vein (Fig. 1).
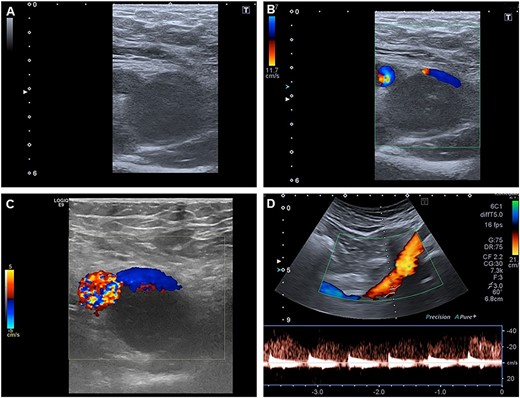
Duplex sonography shows a mass compressing the femoral vein from dorsally.
To clarify the entity of the lesion, MRI-Imaging and a fine needle biopsy were performed. In the MRI, the tumor had a slightly hyperintense signal in the T2-weighted images and a more hypointense signal compared to fat. In the T1-weighted images, the signal of the tumor was comparable to the muscular signal, and after application of contrast medium, a slight enhancement of the tumor was observed (Fig. 2). In the fine needle biopsy, proliferating cells were seen, but no conclusive histological diagnosis could be made.
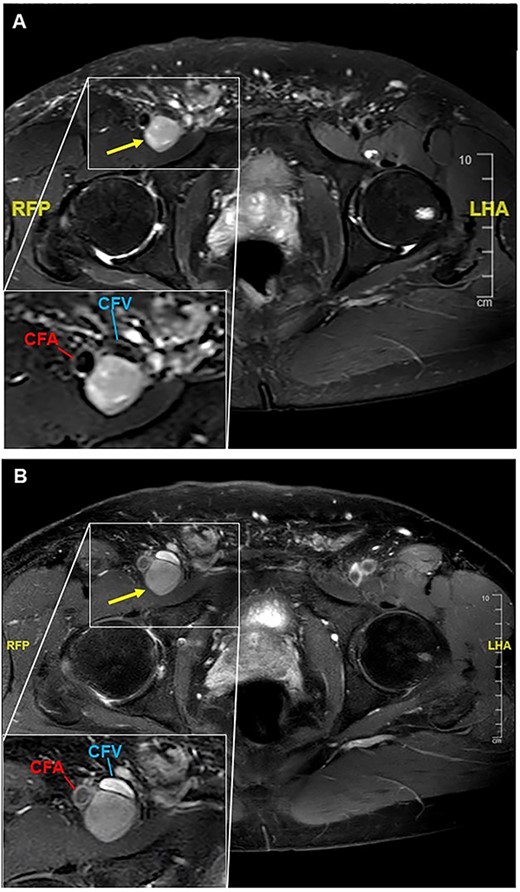
T1-weighted MR-images of the right groin are presented pre- (A) and post-application of contrast medium (B). (A) A tumor with a diameter of 26 × 24 × 54 mm is seen dorsal to the common femoral vein and artery. In the left lower corner, a magnification of the area of interest is shown. CFV = common femoral vein; CFA = common femoral artery. (B) Addition of contrast displays the compression of the common femoral vein, but no flow impairment is seen. In the left lower corner, a magnification of the tumor is presented.
Consequently, the patient was referred to the department of vascular surgery for elective tumor excision. Intraoperatively, we found an elastic tumor compressing the right common femoral vein without infiltration of the surrounding tissue (Fig. 3). The patient recovered well from the surgery and was discharged 2 days later.
List of publications on deep soft tissue leiomyoma affecting the lower extremities.
| No. . | Reference . | Location . | Age (years) . | Sex . |
|---|---|---|---|---|
| 1 | Sengul et al. [4] | Left tibialis anterior muscle | 49 | F |
| 2 | Lopez-Barea et al. [3] | Left calf | 6 | M |
| 3 | Fitzhugh et al. [7] | Right gluteus maximus muscle | 61 | F |
| 4 | Jalgaonkar et al. [8] | Right foot | 5 | M |
| 5 | Watson et al. [10] | Left thigh | 65 | F |
| 6 | Uemura et al. [11] | Thigh | Full-text article not found | |
| 7 | Schmidt-Rohlfing et al. [12] | Right knee | 14 | F |
| 8 | Yamato et al. [13] | Right gluteal muscle | 7 | M |
| 9 | Lee et al. [14] | Right thigh | 42 | M |
| 10 | Horiuchi et al. [15] | Left inguinal region, bilat. thighs, omentum, peritoneum, uterine leiomyomas | 40 | F |
| 11 | Arenas et al. [16] | Right medial gastrocnemius muscle | Full-text article not found | |
| Median (range) | 40 (5 – 65) | |||
| No. . | Reference . | Location . | Age (years) . | Sex . |
|---|---|---|---|---|
| 1 | Sengul et al. [4] | Left tibialis anterior muscle | 49 | F |
| 2 | Lopez-Barea et al. [3] | Left calf | 6 | M |
| 3 | Fitzhugh et al. [7] | Right gluteus maximus muscle | 61 | F |
| 4 | Jalgaonkar et al. [8] | Right foot | 5 | M |
| 5 | Watson et al. [10] | Left thigh | 65 | F |
| 6 | Uemura et al. [11] | Thigh | Full-text article not found | |
| 7 | Schmidt-Rohlfing et al. [12] | Right knee | 14 | F |
| 8 | Yamato et al. [13] | Right gluteal muscle | 7 | M |
| 9 | Lee et al. [14] | Right thigh | 42 | M |
| 10 | Horiuchi et al. [15] | Left inguinal region, bilat. thighs, omentum, peritoneum, uterine leiomyomas | 40 | F |
| 11 | Arenas et al. [16] | Right medial gastrocnemius muscle | Full-text article not found | |
| Median (range) | 40 (5 – 65) | |||
A total of 11 publications were identified. The median age was 40 years. Two articles were not fully available, so no further information about age or sex could be obtained. Of the available articles, five patients were female, and four of male sex.
List of publications on deep soft tissue leiomyoma affecting the lower extremities.
| No. . | Reference . | Location . | Age (years) . | Sex . |
|---|---|---|---|---|
| 1 | Sengul et al. [4] | Left tibialis anterior muscle | 49 | F |
| 2 | Lopez-Barea et al. [3] | Left calf | 6 | M |
| 3 | Fitzhugh et al. [7] | Right gluteus maximus muscle | 61 | F |
| 4 | Jalgaonkar et al. [8] | Right foot | 5 | M |
| 5 | Watson et al. [10] | Left thigh | 65 | F |
| 6 | Uemura et al. [11] | Thigh | Full-text article not found | |
| 7 | Schmidt-Rohlfing et al. [12] | Right knee | 14 | F |
| 8 | Yamato et al. [13] | Right gluteal muscle | 7 | M |
| 9 | Lee et al. [14] | Right thigh | 42 | M |
| 10 | Horiuchi et al. [15] | Left inguinal region, bilat. thighs, omentum, peritoneum, uterine leiomyomas | 40 | F |
| 11 | Arenas et al. [16] | Right medial gastrocnemius muscle | Full-text article not found | |
| Median (range) | 40 (5 – 65) | |||
| No. . | Reference . | Location . | Age (years) . | Sex . |
|---|---|---|---|---|
| 1 | Sengul et al. [4] | Left tibialis anterior muscle | 49 | F |
| 2 | Lopez-Barea et al. [3] | Left calf | 6 | M |
| 3 | Fitzhugh et al. [7] | Right gluteus maximus muscle | 61 | F |
| 4 | Jalgaonkar et al. [8] | Right foot | 5 | M |
| 5 | Watson et al. [10] | Left thigh | 65 | F |
| 6 | Uemura et al. [11] | Thigh | Full-text article not found | |
| 7 | Schmidt-Rohlfing et al. [12] | Right knee | 14 | F |
| 8 | Yamato et al. [13] | Right gluteal muscle | 7 | M |
| 9 | Lee et al. [14] | Right thigh | 42 | M |
| 10 | Horiuchi et al. [15] | Left inguinal region, bilat. thighs, omentum, peritoneum, uterine leiomyomas | 40 | F |
| 11 | Arenas et al. [16] | Right medial gastrocnemius muscle | Full-text article not found | |
| Median (range) | 40 (5 – 65) | |||
A total of 11 publications were identified. The median age was 40 years. Two articles were not fully available, so no further information about age or sex could be obtained. Of the available articles, five patients were female, and four of male sex.
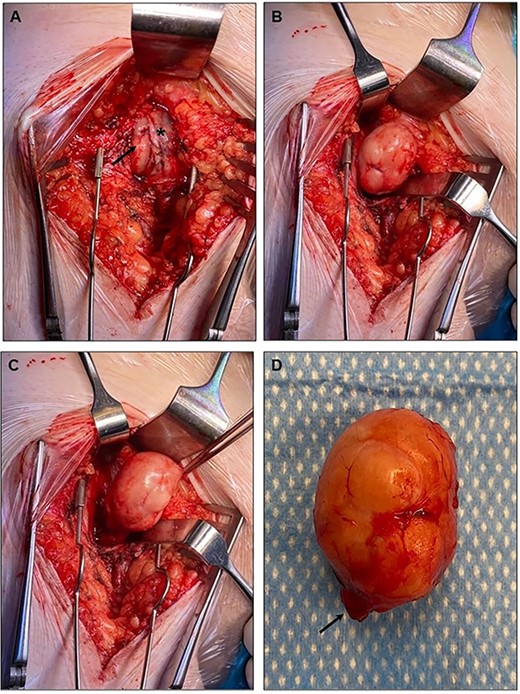
The intraoperative findings are presented. (A) The asterisk indicates the common femoral vein, whereas the arrow indicates the tumor compressing the vein from dorsally. (B, C) Intraoperative preparation steps. (D) Excised tumor. The arrow indicates its vascular supply deriving from the caudal border from the lesion.
The histological examinations (Fig. 4) showed a proliferation of spindle cells resembling smooth muscle cells. The nuclei did not display any signs of atypia and no mitotic activity was observed with <1 mitotic figure in 50 HPF. No necrosis was seen, but single mast cell infiltration. Immunohistochemical staining showed a positivity for smooth muscle actin (SMA) and desmin. Similar findings were described by Ramachandran et al. [9] in a case report of DSTL of the forearm. Interestingly, in our specimen, a low expression of CD34 was discovered. The proliferation index Ki67 did not exceed 5% of the cells. Due to the negativity for expression of mdm2 and beta-catenin, tumors of the spectrum of dedifferentiated liposarcomas or desmoid-fibromatosis were excluded. In summary, DSTL was the most plausible diagnosis even though a low expression of CD34 was seen. Due to the rarity of the findings, the histopathological results were validated in an external, independent pathological institute.
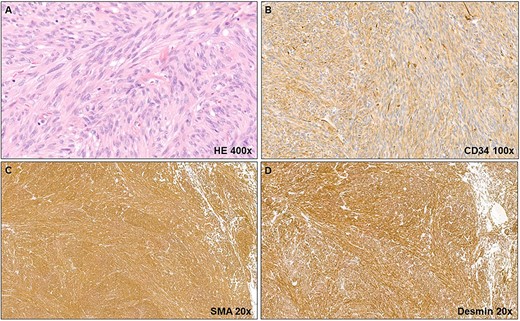
(A) The histopathological examination shows spindle cells (smooth muscle cells) with no mitotic figures or nuclear atypia. Moreover, no necrosis is seen. (B) Immunohistochemical staining reveals a low CD34 expression. (C, D) Further immunohistochemical staining shows positivity for SMA and desmin.
An overview on the case report including the timeline is provided in Fig. 5.
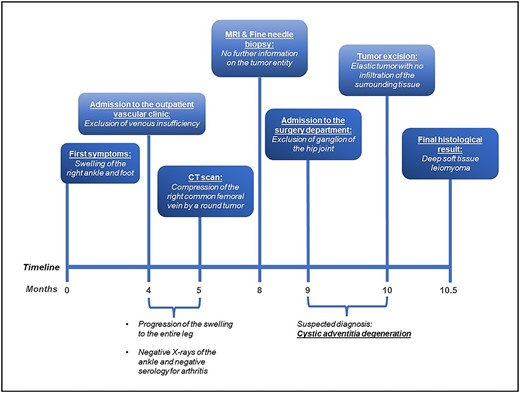
The timeline from first appearance of symptoms to the final diagnosis is represented. Four months after appearance of the first symptoms, swelling of the right ankle and foot, the patient was admitted to the vascular outpatient clinic to exclude venous insufficiency. At this time, duplex sonography of the venous system was unremarkable. After excluding arthritis of the right ankle serologically and radiologically and because of a progression of the edema to the entire leg, a CT scan was performed to exclude pelvic vein thrombosis. A tumor compressing the right common femoral vein was discovered. Significant compression of the venous flow were confirmed by duplex sonography. After 8 months, an MRI and a fine needle biopsy were performed, which provided no further information about the entity of the tumor. After 9 months, the patient was admitted to the surgical department and a month later he was scheduled for tumor excision. The tumor was successfully excised in toto and did not show any signs of infiltration. Histological analysis required external validation due to the rare histological configuration. Two weeks after surgery, deep soft tissue leiomyoma was confirmed. In summary, it took almost one year from initial clinical presentation to the final diagnosis.
Review of literature
Because of the rarity of the tumor entity found, we screened the literature for similar case reports. We inserted the search term “Deep Soft Tissue Leiomyomas” in PubMed and 74 articles published between 1977 and 2021 appeared. Of these articles, publications with no reported cases, articles about leiomyosarcoma, leiomyoma of the uterus or retroperitoneum only and on other tumor entities were excluded. Thirty-five articles were identified and five of them were case series. The selection process is visualized in Fig. 6. In total, DSTL was reported in 65 patients.
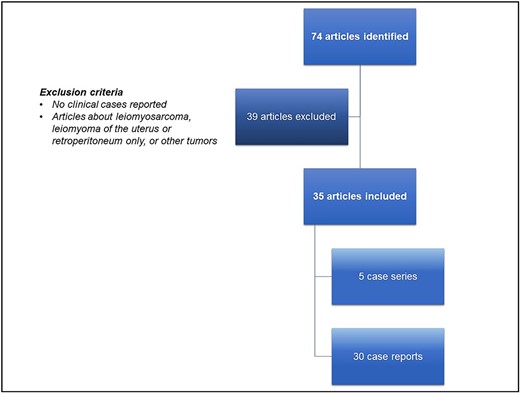
The selection process of the reviewed articles is represented. Of the 74 articles found in PubMed inserting the search term “deep soft tissue leiomyoma”, 39 were excluded according to the exclusion criteria (no clinical cases reported, articles about leiomyosarcoma, leiomyoma of the uterus or retroperitoneum only, or other tumors). Thirty-five articles were included (5 case series and 30 case reports).
The articles were divided into case reports about DSTL of the lower extremities [3, 4, 7, 8, 10–16] (Table 1), upper extremities [2, 9, 17–21, 22] (Table 2), other locations [23–33] (Table 3) and case series [34–38] (Table 4). In summary, of all publications found, the extremities were involved in 35 cases. In total 32 female patients and 29 male patients were reported. The median age range was between 27 and 40 years.
List of publications on deep soft tissue leiomyoma affecting the upper extremities.
| No. . | Reference . | Location . | Age (years) . | Sex . |
|---|---|---|---|---|
| 1 | Misumi et al. [17] | Right elbow | 25 | M |
| 2 | Bommireddy et al. [2] | Right forearm | 25 | F |
| 3 | Yagi et al. [18] | Right deep palmar arterial arch | 65 | F |
| 4 | Ramachandran et al. [9] | Left forearm | 16 | M |
| 5 | Chalidis et al. [19] | Left hand | 32 | M |
| 6 | Hernandez et al. [20] | Right wrist | 6 | F |
| 7 | Paluck et al. [22] | Right wrist | 30 | F |
| 8 | Kim et al. [21] | Left axilla | 29 | M |
| Median (range) | 27 (6 – 65) | |||
| No. . | Reference . | Location . | Age (years) . | Sex . |
|---|---|---|---|---|
| 1 | Misumi et al. [17] | Right elbow | 25 | M |
| 2 | Bommireddy et al. [2] | Right forearm | 25 | F |
| 3 | Yagi et al. [18] | Right deep palmar arterial arch | 65 | F |
| 4 | Ramachandran et al. [9] | Left forearm | 16 | M |
| 5 | Chalidis et al. [19] | Left hand | 32 | M |
| 6 | Hernandez et al. [20] | Right wrist | 6 | F |
| 7 | Paluck et al. [22] | Right wrist | 30 | F |
| 8 | Kim et al. [21] | Left axilla | 29 | M |
| Median (range) | 27 (6 – 65) | |||
A total of eight publications were identified. The median age was 27 years. Four males and four females were affected.
List of publications on deep soft tissue leiomyoma affecting the upper extremities.
| No. . | Reference . | Location . | Age (years) . | Sex . |
|---|---|---|---|---|
| 1 | Misumi et al. [17] | Right elbow | 25 | M |
| 2 | Bommireddy et al. [2] | Right forearm | 25 | F |
| 3 | Yagi et al. [18] | Right deep palmar arterial arch | 65 | F |
| 4 | Ramachandran et al. [9] | Left forearm | 16 | M |
| 5 | Chalidis et al. [19] | Left hand | 32 | M |
| 6 | Hernandez et al. [20] | Right wrist | 6 | F |
| 7 | Paluck et al. [22] | Right wrist | 30 | F |
| 8 | Kim et al. [21] | Left axilla | 29 | M |
| Median (range) | 27 (6 – 65) | |||
| No. . | Reference . | Location . | Age (years) . | Sex . |
|---|---|---|---|---|
| 1 | Misumi et al. [17] | Right elbow | 25 | M |
| 2 | Bommireddy et al. [2] | Right forearm | 25 | F |
| 3 | Yagi et al. [18] | Right deep palmar arterial arch | 65 | F |
| 4 | Ramachandran et al. [9] | Left forearm | 16 | M |
| 5 | Chalidis et al. [19] | Left hand | 32 | M |
| 6 | Hernandez et al. [20] | Right wrist | 6 | F |
| 7 | Paluck et al. [22] | Right wrist | 30 | F |
| 8 | Kim et al. [21] | Left axilla | 29 | M |
| Median (range) | 27 (6 – 65) | |||
A total of eight publications were identified. The median age was 27 years. Four males and four females were affected.
List of publications on deep soft tissue leiomyoma affecting other locations.
| No. . | Reference . | Location . | Age (years) . | Sex . |
|---|---|---|---|---|
| 1 | Batihan et al. [23] | Chest | 26 | F |
| 2 | Sumi et al. [24] | Rectus muscle | 48 | F |
| 3 | Nakamura et al. [25] | Chest | 22 | M |
| 4 | Gallagher et al. [26] | Ischiorectal region | 42 | F |
| 5 | Xu et al. [27] | Scapular region | 34 | M |
| 6 | Hallin et al. [28] | Esophagus | not specified | |
| 7 | El Amine et al. [29] | Abdominal wall hernia sac | full text not available | |
| 8 | Minor et al. [30] | Midline anterior neck | 31 | M |
| 9 | Wang et al. [31] | Middle and lower peritoneal cavity | 22 | M |
| 10 | Kim et al. [32] | Perianal region | 30 | F |
| 11 | Manojlovic et al. [33] | Right pterygoid muscle | 8 | M |
| Median (range) | 30 (8 – 48) | |||
| No. . | Reference . | Location . | Age (years) . | Sex . |
|---|---|---|---|---|
| 1 | Batihan et al. [23] | Chest | 26 | F |
| 2 | Sumi et al. [24] | Rectus muscle | 48 | F |
| 3 | Nakamura et al. [25] | Chest | 22 | M |
| 4 | Gallagher et al. [26] | Ischiorectal region | 42 | F |
| 5 | Xu et al. [27] | Scapular region | 34 | M |
| 6 | Hallin et al. [28] | Esophagus | not specified | |
| 7 | El Amine et al. [29] | Abdominal wall hernia sac | full text not available | |
| 8 | Minor et al. [30] | Midline anterior neck | 31 | M |
| 9 | Wang et al. [31] | Middle and lower peritoneal cavity | 22 | M |
| 10 | Kim et al. [32] | Perianal region | 30 | F |
| 11 | Manojlovic et al. [33] | Right pterygoid muscle | 8 | M |
| Median (range) | 30 (8 – 48) | |||
A total of 11 publications were identified. The median age was 30 years, and five male and four female patients were affected. In two publications, no sex- or age-related data could be found.
List of publications on deep soft tissue leiomyoma affecting other locations.
| No. . | Reference . | Location . | Age (years) . | Sex . |
|---|---|---|---|---|
| 1 | Batihan et al. [23] | Chest | 26 | F |
| 2 | Sumi et al. [24] | Rectus muscle | 48 | F |
| 3 | Nakamura et al. [25] | Chest | 22 | M |
| 4 | Gallagher et al. [26] | Ischiorectal region | 42 | F |
| 5 | Xu et al. [27] | Scapular region | 34 | M |
| 6 | Hallin et al. [28] | Esophagus | not specified | |
| 7 | El Amine et al. [29] | Abdominal wall hernia sac | full text not available | |
| 8 | Minor et al. [30] | Midline anterior neck | 31 | M |
| 9 | Wang et al. [31] | Middle and lower peritoneal cavity | 22 | M |
| 10 | Kim et al. [32] | Perianal region | 30 | F |
| 11 | Manojlovic et al. [33] | Right pterygoid muscle | 8 | M |
| Median (range) | 30 (8 – 48) | |||
| No. . | Reference . | Location . | Age (years) . | Sex . |
|---|---|---|---|---|
| 1 | Batihan et al. [23] | Chest | 26 | F |
| 2 | Sumi et al. [24] | Rectus muscle | 48 | F |
| 3 | Nakamura et al. [25] | Chest | 22 | M |
| 4 | Gallagher et al. [26] | Ischiorectal region | 42 | F |
| 5 | Xu et al. [27] | Scapular region | 34 | M |
| 6 | Hallin et al. [28] | Esophagus | not specified | |
| 7 | El Amine et al. [29] | Abdominal wall hernia sac | full text not available | |
| 8 | Minor et al. [30] | Midline anterior neck | 31 | M |
| 9 | Wang et al. [31] | Middle and lower peritoneal cavity | 22 | M |
| 10 | Kim et al. [32] | Perianal region | 30 | F |
| 11 | Manojlovic et al. [33] | Right pterygoid muscle | 8 | M |
| Median (range) | 30 (8 – 48) | |||
A total of 11 publications were identified. The median age was 30 years, and five male and four female patients were affected. In two publications, no sex- or age-related data could be found.
| No. . | Reference . | Cases no. . | Location . | Age (years, median (range)) . | Sex . |
|---|---|---|---|---|---|
| 1 | Kilpatrick et al. [34] | 11 | 5 extremities, 6 other | 35 (14 - 62) | 5 F, 6 M |
| 2 | Billings et al. [35] | 16 | 7 lower extremities, 3 mesentery, 2 upper extremities, 1 rectus abdominis muscle, 1 chest wall, 1 axilla, 1 shoulder | 39 (6 - 55) | 8 F, 8 M |
| 3 | Herrlin et al. [36] | 4 | 2 thigh, 1 ischiorectal fossa, 1 supraclavicular region | 25 (19 - 74) | 2 F, 2 M |
| 4 | Montague et al. [37] | 2 | 2 oral cavity | 35 (18, 51) | 2 F |
| 5 | Adamicova et al. [38] | 2 | 1 head, 1 perineum | 53 (43, 63) | 2 F |
| Median (range) | 37 (6 – 74) | ||||
| No. . | Reference . | Cases no. . | Location . | Age (years, median (range)) . | Sex . |
|---|---|---|---|---|---|
| 1 | Kilpatrick et al. [34] | 11 | 5 extremities, 6 other | 35 (14 - 62) | 5 F, 6 M |
| 2 | Billings et al. [35] | 16 | 7 lower extremities, 3 mesentery, 2 upper extremities, 1 rectus abdominis muscle, 1 chest wall, 1 axilla, 1 shoulder | 39 (6 - 55) | 8 F, 8 M |
| 3 | Herrlin et al. [36] | 4 | 2 thigh, 1 ischiorectal fossa, 1 supraclavicular region | 25 (19 - 74) | 2 F, 2 M |
| 4 | Montague et al. [37] | 2 | 2 oral cavity | 35 (18, 51) | 2 F |
| 5 | Adamicova et al. [38] | 2 | 1 head, 1 perineum | 53 (43, 63) | 2 F |
| Median (range) | 37 (6 – 74) | ||||
A total of five case series were identified. In the case series of Billings et al., a total of 36 cases were presented, but according to our exclusion criteria, we excluded 20 of the reported cases due to their location in the retroperitoneum. In total, 35 cases were reported and 16 affected the extremities. The median age was 37 years. 19 female and 16 male patients were affected.
| No. . | Reference . | Cases no. . | Location . | Age (years, median (range)) . | Sex . |
|---|---|---|---|---|---|
| 1 | Kilpatrick et al. [34] | 11 | 5 extremities, 6 other | 35 (14 - 62) | 5 F, 6 M |
| 2 | Billings et al. [35] | 16 | 7 lower extremities, 3 mesentery, 2 upper extremities, 1 rectus abdominis muscle, 1 chest wall, 1 axilla, 1 shoulder | 39 (6 - 55) | 8 F, 8 M |
| 3 | Herrlin et al. [36] | 4 | 2 thigh, 1 ischiorectal fossa, 1 supraclavicular region | 25 (19 - 74) | 2 F, 2 M |
| 4 | Montague et al. [37] | 2 | 2 oral cavity | 35 (18, 51) | 2 F |
| 5 | Adamicova et al. [38] | 2 | 1 head, 1 perineum | 53 (43, 63) | 2 F |
| Median (range) | 37 (6 – 74) | ||||
| No. . | Reference . | Cases no. . | Location . | Age (years, median (range)) . | Sex . |
|---|---|---|---|---|---|
| 1 | Kilpatrick et al. [34] | 11 | 5 extremities, 6 other | 35 (14 - 62) | 5 F, 6 M |
| 2 | Billings et al. [35] | 16 | 7 lower extremities, 3 mesentery, 2 upper extremities, 1 rectus abdominis muscle, 1 chest wall, 1 axilla, 1 shoulder | 39 (6 - 55) | 8 F, 8 M |
| 3 | Herrlin et al. [36] | 4 | 2 thigh, 1 ischiorectal fossa, 1 supraclavicular region | 25 (19 - 74) | 2 F, 2 M |
| 4 | Montague et al. [37] | 2 | 2 oral cavity | 35 (18, 51) | 2 F |
| 5 | Adamicova et al. [38] | 2 | 1 head, 1 perineum | 53 (43, 63) | 2 F |
| Median (range) | 37 (6 – 74) | ||||
A total of five case series were identified. In the case series of Billings et al., a total of 36 cases were presented, but according to our exclusion criteria, we excluded 20 of the reported cases due to their location in the retroperitoneum. In total, 35 cases were reported and 16 affected the extremities. The median age was 37 years. 19 female and 16 male patients were affected.
Discussion
Here we reported a case of DSTL of the groin with initially misleading symptoms. It took several diagnostic steps to find the tumor and to confirm the tumor entity.
The fine needle biopsy was negative. This sometimes happens also in malignant tumors. Thus, if a malignant tumor is suspected, the surgical approach must be thoroughly planned and if re-operation is required, the excision/biopsy canal must be removed. Moreover, further full-body imaging must be performed to exclude metastasis.
Klijanienko et al. [39] undermines the importance of keeping in mind possible differential diagnoses of histological detection of leiomyosarcoma, such as leiomyoma, malignant peripheral nerve sheath tumor, monophasic synovial sarcoma, and malignant fibrous histiocytoma. In this regard, aspiration biopsy has been described a reliable tool to appropriately distinguish even well differentiated leiomyosarcoma from leiomyoma [40].
DSTL are rare tumors that require thorough histopathological examination for correct diagnosis. Significant cell atypia, high mitotic rate and coagulative tumor necrosis need to be excluded [35, 41] like in our specimen. Billings et al. highlight the importance of stringent histologic criteria by which accurate diagnosis is assured [7]. Actin or desmin staining can show the presence of smooth muscle. However, histologic criteria are inconsistently applied and smooth muscle tumors’ growth behavior is hardly predictable [42]. According to Goodman and Briggs [43], they originate from undifferentiated mesenchymal cells or smooth muscle cell rests, whereas other authors claim they originate from smooth muscle cells in the walls of blood vessels [44]. The tumors can be further classified into vascular and non-vascular [2].
Due to their rare occurrence, an imaging-based diagnosis is almost impossible, even by MRI [17]. In the reported cases of literature, differential diagnosis included myositis ossificans [1, 2, 43], calcific myonecrosis, [7] and chondrogenic tumor [45] due to the presence of scattered calcifications [43] and/or ossification [7]. In fact, calcification occurs in approximately one third of cases [1]. Further differential diagnoses were Ewing sarcoma [2], lipoma, leiomyosarcoma, schwannoma, neurofibroma, hemangioma, and soft-tissue giant-cell tumor of the tendon [9]. In our case, differential diagnosis included arthritis due to the initial isolated swelling of the ankle and foot. Only when the swelling progressed, the entire leg and inguinal region were examined.
Localization of DSTL in the upper extremities is less common than in the lower extremities [16]. Most cases on affection of the upper extremities were discovered because patients referred pain or swelling due to the tumor’s growth [2, 17]. Beside the extremities, different locations of leiomyoma have been described such as of the gallbladder [46], of the anterior neck [30], of the sternothyroid muscle [47], of the pterygoid muscle [33], of the head and the perineum [38], gastric leiomyoma [48–51], tracheal and bronchial leiomyoma [52–56].
Usually, diagnosis is secured only after tumor excision. In most of the reported cases, no tumor occurrence was described after surgery [1, 2, 4, 16, 30, 57]. Nevertheless, Adamicová et al. [38] described recurrence of a leiomyoma after 5 years in one patient. However, malignant transformation hardly occurs [57]. Despite their benign entity, “benign metastasizing leiomyomas” have been described by Horiuchi et al. [15] and Rivera et al. [58]
Kilpatrick et al. [34] described a series of patients with DSTL and most of them had their tumors located in the extremities (5/11 cases). Although cell atypia is an exclusion criterium, in this case series, degenerative nuclear changes were found [34]. However, in concordance with the histological criteria none of the specimens exceeded one mitotic figure per 50 high-power fields [34].
Conclusion
DSTL are rare tumors mainly found in the uterus. The size and the location of the tumor determine the symptoms of the patient. Imaging with CT-Scans, MRI and ultrasound should not be performed to confirm the diagnosis but to determine the exact location of the tumor and to rule out any other neoplasia. From a surgical point of view, it is important to plan the biopsy canal in a way that if needed, it can be excised during the final tumor resection. Preoperative presentation in a sarcoma board might be beneficial to have a multidisciplinary team involved, to share their expertise on these rare cases and to find the best treatment options for the individual patient.
Author contributions
F.N.: Data Curation, Writing – Original Draft; I.Z.: Conceptualization, Data Curation, Writing – Original Draft, Writing – Review and Editing, Visualization; J.A.: Visualization, Writing – Review and Editing; S.S.: Data Curation, Visualization, Writing – Review and Editing; R.M.: Supervision, Data Curation, Writing – Review and Editing.
Conflict of interest statement
None declared.
Funding
None declared.
References
Author notes
Falk Nessenius and Isabel Zucal share the co-first authorship of this work.



