-
PDF
- Split View
-
Views
-
Cite
Cite
Samantha Jolly, Nikhil Kundu, Suraj Rathnayake, A case of mistaken identity: bile duct masquerading as gallbladder, Journal of Surgical Case Reports, Volume 2023, Issue 1, January 2023, rjad001, https://doi.org/10.1093/jscr/rjad001
Close - Share Icon Share
Abstract
Laparoscopic cholecystectomy is a common surgical procedure, with potential for significant morbidity. The incidence of bile duct injuries has increased with the advent of laparoscopy, occurring in up to 1% of cases. Risk of injury increases with aberrant anatomy, acute inflammation and fibrosis. Preventative strategies include obtaining the critical view of safety, using a fundus-first approach and performing a subtotal cholecystectomy in the difficult gallbladder. Although controversy exists for routine cholangiography, its use is helpful in situations of obscure anatomy. We describe the case of a chronically inflamed and unusually small 1.5 cm gallbladder with an obliterated cystic duct. The critical view of safety was not able to be achieved and intraoperative cholangiography enabled identification of aberrant anatomy, with a dilated common duct mistaken as the gallbladder infundibulum. This case highlights the need to be vigilant to structural variation and the utility of selective cholangiography to clarify anatomy.
INTRODUCTION
Laparoscopic cholecystectomy is one of the most common general surgical operations in the elective and emergency setting [1, 2]. Iatrogenic bile duct injuries (BDI) represent a considerable cause of morbidity, occurring in ∼0.5–1% of cases and often needing endoscopic or operative intervention [3]. Their incidence has increased with the advent of laparoscopy and is further heightened in the presence of aberrant anatomy, acute inflammation and fibrosis [2]. Achieving the critical view of safety is not always possible, and other preventative techniques such as a fundus-first approach, subtotal cholecystectomy and intraoperative cholangiogram should be considered [4]. We describe the case of aberrant biliary anatomy with a small, contracted gallbladder and no discernible cystic duct. A fundus-first approach and cholangiography enabled identification of anatomy and prevention of a major BDI. The consequence was a minor BDI treated endoscopically.
CASE REPORT
A 38-year-old female presented for an elective laparoscopic cholecystectomy on a background of previous cholecystitis. She had not had any previous abdominal surgeries, and her medical history consists of chronic hepatitis B and obesity. Preoperative abdominal ultrasonography demonstrated a contracted gallbladder with gallstones, and a difficult-to-appreciate common bile duct which did not appear dilated.
Intraoperatively, the biliary anatomy was distorted by chronic inflammatory change, and a critical view of safety was not able to be achieved. When attempting to clear the hepatocystic triangle, a window was made around the structure believed to be the gallbladder infundibulum. There was no artery identified entering the gallbladder. To help facilitate identification of structures, a cholangiogram was performed. A ductotomy was made with laparoscopic scissors below the infundibulum presumed to be cystic duct, and a catheter inserted into the duct which was secured with a cholangiography clamp. About 20 mL of 50–50 mixture of saline and iodinated contrast was injected under fluoroscopy (Fig. 1). This revealed proximal filling with hepatic trifurcation from a common confluence, and distal flow into the duodenum without evidence of a cystic duct, and thus identified a ductotomy through the common bile duct. A second surgeon was called into the operating theatre for confirmation of findings, and the ductotomy was closed laparoscopically with Polydioxanone (PDS) sutures. ‘Fundus first’ dissection revealed a small 1.5 cm gallbladder and confirmed no discernible cystic duct (Fig. 2). There was no impacted stone to suggest a Mirizzi syndrome. A PDS endoloop was placed around the gallbladder at the junction of the bile duct, and a drain placed in the subhepatic space. Figure 3 demonstrates the small operative specimen.

The patient was up transferred to the regional tertiary centre where endoscopic retrograde cholangiopancreatography (ERCP) was performed with sphincterotomy and biliary stenting. Hedrain was removed after ERCP, and she returned 6 weeks later for repeat ERCP and removal of stent. She remains well at 4-month follow-up.
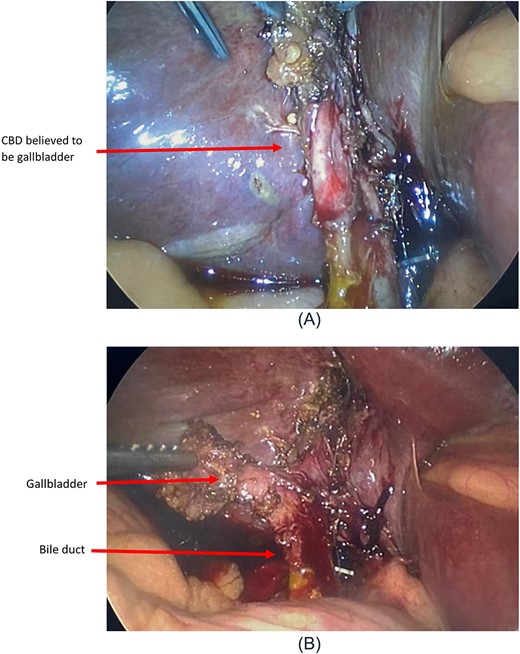
(A) Intraoperative view following cholangiogram. (B) Intraoperative view following fundus-first approach.

DISCUSSION
BDI during laparoscopic cholecystectomy remains a serious complication with significant postoperative sequelae in the short and long term [2]. This occurs in up to 1% of patients and represents an important cause of morbidity and mortality [2]. The ‘critical view of safety’ was introduced in 1995 as a means of preventing iatrogenic BDI through avoiding misidentification of the main bile duct [5]. There are three components to obtaining this view: clear Calots triangle of fat and fibrous tissue, clear the lower part of the gallbladder from the cystic plate and isolate only two structures entering the gallbladder [5]. However, in the presence of severe inflammation, BDI are more likely to occur, often from mistaking the common bile duct as the cystic duct following circumferential dissection—the ‘hidden cystic duct’ syndrome [6]. Conversion to open does not always improve visibility in cases of a precarious hepatocystic triangle [4]. A useful extrabiliary anatomical landmark, present in 68–90% of patients, is ‘Rouviere’s sulcus’ between the right lobe of liver and caudate process, with dissection commencing above this to avoid the common bile duct [1, 7].
Routine intraoperative cholangiogram is not yet recommended, however is useful in cases where the critical view is unable to be achieved, there is a suspicion of BDI or unclear anatomy [2]. In this case, cholangiography enabled identification of aberrant anatomy, with a small gallbladder and obliterated cystic duct, and ultimately prevented a major BDI. The consequence was a minor BDI with minimal tissue loss, managed via direct repair and drainage, as per standard recommendations for minor BDI (Strasberg A-D) [2].
Antegrade dissection (i.e. fundus first) can be used for the difficult gallbladder, with other safe methods including a subtotal cholecystectomy or conversion to open. Through a subsequent antegrade dissection, a 1.5 cm gallbladder was identified, where usual dimensions are up to 10 cm length. Gallbladder anomalies are rare, with aberrant and ectopic gallbladders occurring in 0.3–0.7% of the population [8]. This case highlights the importance of remaining vigilant to biliary variants, with selective use of cholangiography to aid safe cholecystectomy.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



