-
PDF
- Split View
-
Views
-
Cite
Cite
Awadh Alqahtani, Mohammad Almayouf, Srikar Billa, Omar Alsarraj, Albandry Bin Zamil, A splenic pseudocyst following laparoscopic sleeve gastrectomy: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 1, January 2023, rjac624, https://doi.org/10.1093/jscr/rjac624
Close - Share Icon Share
Abstract
This is the first report of a patient presenting with a splenic pseudocyst following laparoscopic sleeve gastrectomy (LSG). A 26-year-old male with no chronic medical illnesses who underwent LSG presented with vague abdominal pain. An abdominal contrast-enhanced computed tomography revealed a 15 cm well-circumscribed cyst originating from the spleen. Intraoperatively, the findings were significant for a superficial cyst located at the lower pole of the spleen. A laparoscopic spleen-preserving procedure was conducted, specifically marsupialization and packing with omentum. The postoperative period was uneventful, and the patient was discharged on Day 2 postoperatively. The patient was free from complaints at outpatient follow-up clinics. Follow-up visits at the outpatient clinic were free from complaints. Pathology confirmed a splenic pseudocyst, and cytology was unremarkable. Since dissection during LSG is close to the spleen, infarction could occur, predisposing to pseudocyst formation. Marsupialization is an excellent surgical option when applied to appropriate splenic cyst types.
INTRODUCTION
Splenic pseudocysts are uncommonly reported in the literature. Although there is no consensus, the leading theory of pseudocyst development has a prior history of trauma leading to its development. Management of these cysts ranged from conservative observation to complete splenic resection [1]. To our knowledge, no report mentioned the management of splenic pseudocyst after laparoscopic sleeve gastrectomy (LSG).
CASE PRESENTATION
The patient is a 26-year-old male with no chronic medical illnesses who underwent LSG 1 year before his presentation. He presented to the emergency department complaining of intermittent abdominal pain for 4 days. The patient reported feeling fullness in the left upper quadrant area and denied any recent history of abdominal trauma. Examination revealed a swelling at the left upper quadrant. Laboratory investigations were unremarkable. Contrast-enhanced computed tomography showed a large septated cystic lesion of 10 cm compressing the left kidney (Fig. 1). A magnetic resonance image confirmed a non-enhancing cyst with internal septations (Fig. 2). Several factors made us offer laparoscopic exploration and cyst removal to the patient, including the reported symptoms, the cyst size and to confirm the nature of the cyst.
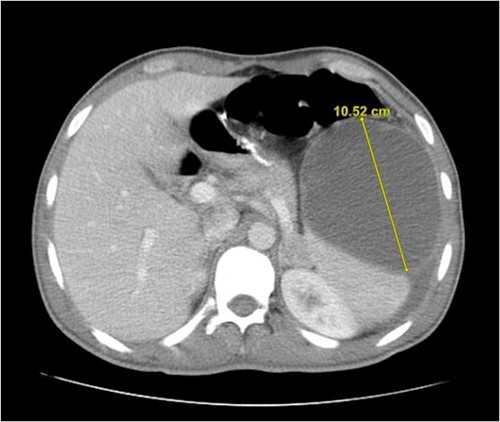
An abdominal contrast-enhanced computed tomography showing a cyst originating from spleen
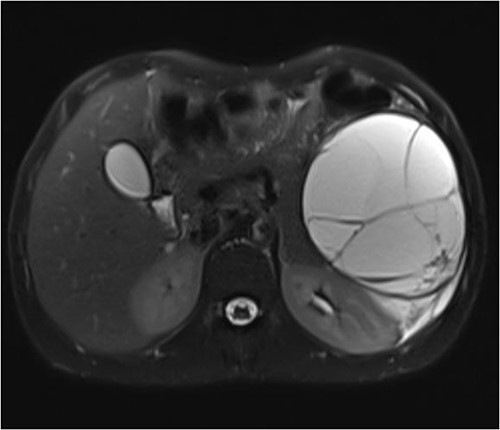
T2 abdominal contrast magnetic resonance image showing the cyst
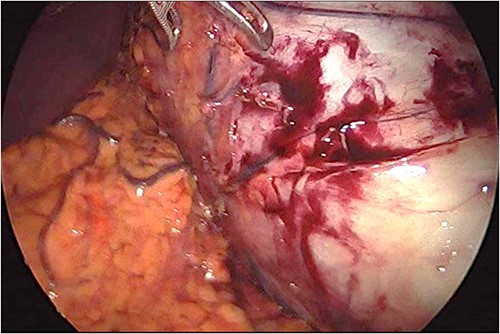
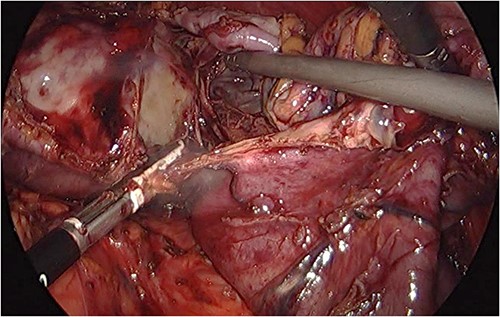
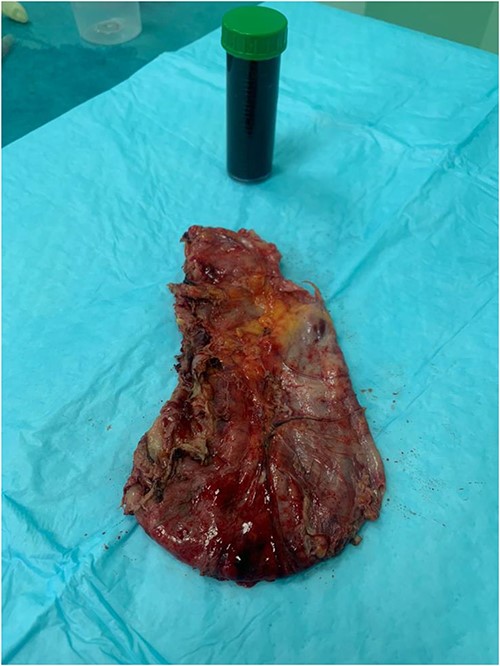
Preoperative prophylactic antibiotics and anticoagulant were given upon induction of anesthesia. The abdomen was accessed safely using a 5-mm vesiport under the guidance of the camera to the left and above the umbilicus. The remaining ports, a 15-mm port 5 cm at the right and above the umbilicus, a 5-mm ports at the left upper quadrant and 5-mm ports at the right upper quadrant were placed with no issues. The cyst was located at the lower pole of the spleen (Fig. 3). The operation consisted of opening the cyst and aspirating dark fluid, removal of the cyst wall (Fig. 4), cauterizing the part of the cyst adherent to the spleen, packing the surgical area with the omentum and removal of the specimen (Fig. 5). The postoperative period was uneventful. The final pathology showed a cyst wall lacking epithelial lining confirming the diagnosis of a pseudocyst, and the cystic fluid showed no malignant cells.
DISCUSSION
Splenic cysts can be classified according to their origin and pathogenesis. It can be considered primary if there is no external causative agent and more congenital in origin. The secondary splenic cysts appear to be related to trauma or infarcts [1]. From a histopathology standpoint, the cyst wall lacking epithelium is almost conclusive and a prerequisite to label a cyst as pseudocyst secondary to an insult [2]. The proximity of dissection during LSG is a potential risk factor for partial splenic infarcts or injury hence predisposing to the formation of a secondary splenic cyst [3].
The presentation of a splenic cyst can be miscellaneous, from being asymptomatic and discovered incidentally, to having vague abdominal pain, to an emergency presentation because of rupture and hemoperitoneum [4–6]. Abdominal imaging is the mainstay of investigation and preferably be a contrast-enhanced image with computed tomography or magnetic resonance imaging to rule out potentially malignant lesions [7].
Different surgical options for managing splenic pseudocysts were mentioned in the literature. It ranged from the least-invasive drainage to total splenectomy and cystectomy (Table 1).
| Author . | Number of patients . | Maximum dimension . | Management . | Complications . |
|---|---|---|---|---|
| Matsutani et al. [5] | 1 | 10.5 cm | Laparoscopic unroofing | None |
| Verma et al. [8] | 2 | 32 cm 12 cm | Open splenectomy; Open cystectomy | NA |
| Galyfos et al. [9] | 2 | 10 cm 7 cm | Laparoscopic splenectomy; Open splenectomy | None |
| Cormican et al. [10] | 1 | 40 cm | Open cystectomy | None |
| Anjuma et al. [11] | 1 | 4.8 cm | Laparoscopic marsupialization | None |
| Sarwal et al. [12] | 1 | 14 cm | Laparoscopic splenectomy | None |
| Author . | Number of patients . | Maximum dimension . | Management . | Complications . |
|---|---|---|---|---|
| Matsutani et al. [5] | 1 | 10.5 cm | Laparoscopic unroofing | None |
| Verma et al. [8] | 2 | 32 cm 12 cm | Open splenectomy; Open cystectomy | NA |
| Galyfos et al. [9] | 2 | 10 cm 7 cm | Laparoscopic splenectomy; Open splenectomy | None |
| Cormican et al. [10] | 1 | 40 cm | Open cystectomy | None |
| Anjuma et al. [11] | 1 | 4.8 cm | Laparoscopic marsupialization | None |
| Sarwal et al. [12] | 1 | 14 cm | Laparoscopic splenectomy | None |
| Author . | Number of patients . | Maximum dimension . | Management . | Complications . |
|---|---|---|---|---|
| Matsutani et al. [5] | 1 | 10.5 cm | Laparoscopic unroofing | None |
| Verma et al. [8] | 2 | 32 cm 12 cm | Open splenectomy; Open cystectomy | NA |
| Galyfos et al. [9] | 2 | 10 cm 7 cm | Laparoscopic splenectomy; Open splenectomy | None |
| Cormican et al. [10] | 1 | 40 cm | Open cystectomy | None |
| Anjuma et al. [11] | 1 | 4.8 cm | Laparoscopic marsupialization | None |
| Sarwal et al. [12] | 1 | 14 cm | Laparoscopic splenectomy | None |
| Author . | Number of patients . | Maximum dimension . | Management . | Complications . |
|---|---|---|---|---|
| Matsutani et al. [5] | 1 | 10.5 cm | Laparoscopic unroofing | None |
| Verma et al. [8] | 2 | 32 cm 12 cm | Open splenectomy; Open cystectomy | NA |
| Galyfos et al. [9] | 2 | 10 cm 7 cm | Laparoscopic splenectomy; Open splenectomy | None |
| Cormican et al. [10] | 1 | 40 cm | Open cystectomy | None |
| Anjuma et al. [11] | 1 | 4.8 cm | Laparoscopic marsupialization | None |
| Sarwal et al. [12] | 1 | 14 cm | Laparoscopic splenectomy | None |
Percutaneous drainage has been utilized because of its less invasive nature and the ability to preserve the spleen. Unfortunately, this method is accompanied by an unacceptable rate of recurrence. [13] A more aggressive approach with total splenectomy and cystectomy is evident in the literature, especially for relatively large cysts [8, 10]. Although not typical, the downside of total splenectomy is the risk of overwhelming post-splenectomy infection, the need for attention to the risks of infection and routine immunization [14]. Partial splenectomy can be offered to preserve the spleen, but it is technically demanding and could be converted to total splenectomy if a large portion gets infarcted and cannot be salvaged [15, 16].
Spleen-preserving procedures offer to remove the cyst and avoid spleen resection. Marsupialization, deroofing and decapsulation are the main options stated in the literature [1]. Some authors did not concur with these procedures as they pose a potential risk of recurrence. After reviewing reports in the literature stating cyst recurrence following spleen-preserving procedures, some cyst features have a higher chance of recurrence than others (Table 2).
| Author . | Number of patients . | Type of procedure . | Recurrence . | Pathology . |
|---|---|---|---|---|
| Palanivelu et al. [17] | 3 | Marsupialization | 2 | 2 mesothelial |
| Mertens et al. [18] | 7 | Decapsulation | 1 | 1 primary cyst |
| Fisher et al. [19] | 8 | Cyst excision | 7 | 6 epidermoid cyst 1 pseudocyst |
| Czauderna et al. [20] | 9 | Fenestration and deroofing | 4 | 4 epidermoid |
| Chin et al. [16] | 9 | Unroofing and decapsulation | 3 | 2 epithelial 1 pseudocyst |
| Ganti et al. [21] | 2 | Marsupialization | 2 | 2 true cysts |
| Author . | Number of patients . | Type of procedure . | Recurrence . | Pathology . |
|---|---|---|---|---|
| Palanivelu et al. [17] | 3 | Marsupialization | 2 | 2 mesothelial |
| Mertens et al. [18] | 7 | Decapsulation | 1 | 1 primary cyst |
| Fisher et al. [19] | 8 | Cyst excision | 7 | 6 epidermoid cyst 1 pseudocyst |
| Czauderna et al. [20] | 9 | Fenestration and deroofing | 4 | 4 epidermoid |
| Chin et al. [16] | 9 | Unroofing and decapsulation | 3 | 2 epithelial 1 pseudocyst |
| Ganti et al. [21] | 2 | Marsupialization | 2 | 2 true cysts |
| Author . | Number of patients . | Type of procedure . | Recurrence . | Pathology . |
|---|---|---|---|---|
| Palanivelu et al. [17] | 3 | Marsupialization | 2 | 2 mesothelial |
| Mertens et al. [18] | 7 | Decapsulation | 1 | 1 primary cyst |
| Fisher et al. [19] | 8 | Cyst excision | 7 | 6 epidermoid cyst 1 pseudocyst |
| Czauderna et al. [20] | 9 | Fenestration and deroofing | 4 | 4 epidermoid |
| Chin et al. [16] | 9 | Unroofing and decapsulation | 3 | 2 epithelial 1 pseudocyst |
| Ganti et al. [21] | 2 | Marsupialization | 2 | 2 true cysts |
| Author . | Number of patients . | Type of procedure . | Recurrence . | Pathology . |
|---|---|---|---|---|
| Palanivelu et al. [17] | 3 | Marsupialization | 2 | 2 mesothelial |
| Mertens et al. [18] | 7 | Decapsulation | 1 | 1 primary cyst |
| Fisher et al. [19] | 8 | Cyst excision | 7 | 6 epidermoid cyst 1 pseudocyst |
| Czauderna et al. [20] | 9 | Fenestration and deroofing | 4 | 4 epidermoid |
| Chin et al. [16] | 9 | Unroofing and decapsulation | 3 | 2 epithelial 1 pseudocyst |
| Ganti et al. [21] | 2 | Marsupialization | 2 | 2 true cysts |
A cyst located internally has a higher chance of recurrence because of possible incomplete cyst removal [21]. If the pathology came to be a primary/true cyst, the chance of recurrence is significant with spleen-preserving procedures. Additionally, true cysts adjacent to other structures (e.g. diaphragm) bear a higher chance of recurrence because of possible epithelization and fluid re-accumulation [16].
CONCLUSION
With trauma/splenic infarct being the primary pathophysiology behind pseudocyst formation, splenic pseudocyst could develop following LSG. Managing a superficially located pseudocyst with a spleen-preserving procedure is an acceptable, safe option and confers a relatively low recurrence rate.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
AUTHORS’ CONTRIBUTIONS
Dr Awadh Alqahtani: concept and review.
Dr Mohammad Almayouf: writing and literature review.
Dr Srikar Billa: acquiring images.
Dr Omar Alsarraj: acquiring images.
Dr Albandary Bin Zamil: writing and acquiring images.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
Morgenstern L. Nonparasitic splenic cysts: pathogenesis, classification, and treatment.
- abdominal pain
- computed tomography
- cytology
- ambulatory care facilities
- cysts
- tissue dissection
- follow-up
- infarction
- laparoscopy
- omentum
- outpatients
- surgical procedures, operative
- abdomen
- pathology
- spleen
- pseudocyst
- cyst of spleen
- marsupialization
- follow-up visit
- sleeve gastrectomy, laparoscopic
- splenic pseudocyst



