-
PDF
- Split View
-
Views
-
Cite
Cite
Héctor Joaquín Pérez Corzo, Angélica Katherine Romero Suárez, Roberto Esau Salgado Salas, Felipe Nieto Segura, José Sergio Verboonen Sotelo, Jeffry Romero Manzano, José Aldo Guzmán Barba, Isaac Esparza Estrada, Unexpected finding of leiomyoma during laparoscopic gastric sleeve: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 1, January 2023, rjac626, https://doi.org/10.1093/jscr/rjac626
Close - Share Icon Share
Abstract
Obesity is a chronic disease with pandemic levels of prevalence worldwide. The most often performed bariatric procedure is sleeve gastrectomy. Although the patient’s history may not indicate preoperative imaging studies, coincidental findings of unexpected pathology are not uncommon, such as leiomyoma. A 41-year-old female was scheduled to laparoscopic gastric sleeve with no contraindications for surgery. A tumor-like mass was identified on the left lateral face of the distal third of the esophagus. Trans-surgical endoscopy and pneumatic test were performed to rule out any type of communication. The surgeon managed to remove the tumor mass, that was sent to histopathological study, and concluded the procedure without complications. Benign tumors of the esophagus are rarely found lesions. Occasionally unexpected findings may occur during surgery, and they should be resolved intraoperatively when possible to allow the completion of the originally planned surgical procedure.
INTRODUCTION
Obesity is a multifaceted, chronic illness with pandemic levels of prevalence worldwide [1]. The most successful method of treating obesity is bariatric surgery. Additionally, it significantly increases the remission rate and improvement of metabolic co-morbidities [2]. The most often performed bariatric procedure in the world is laparoscopic vertical sleeve gastrectomy [3].
The prevalence of morbid obesity is rising and so is the number of bariatric surgeries carried out. Today, laparoscopy is the primary method used in all bariatric surgeries. Although the patient’s history may not indicate preoperative examinations, coincidental findings of unexpected pathology are not uncommon [4]. Submucosal growth, known as gastric leiomyoma, represents 2.5% of stomach tumors. It can be intraluminal or extramural, most frequently occurring in patients between 20 and 50 years old. Most common in the distal two-thirds of the esophagus, where they typically develop intramurally. The majority of them generally have no symptoms and are traditionally manifested as a filling malformation of the stomach wall and are seen as a submucosal mass during endoscopy. Gastric leiomyomectomy is the recommended course of treatment for these lesions [5].
CASE REPORT
A 41-year-old female patient, originally from and a resident of the USA, was scheduled to undergo laparoscopic gastric sleeve surgery; her height = 1.70 m, weight = 114 kg, body mass index = 39.4, with a history of arterial hypertension of 4 years of evolution, which was controlled with amlodipine, depression and anxiety of 26 years of evolution without treatment. Surgical background included three cesarean sections; the last one was 10 years ago, and hysterectomy was done 6 years ago. There was no further history of importance. The patient reported multiple diet and exercise regimens as well as the use of phentermine with no results. Pre-surgical assessment was performed with no contraindications for surgery. Laboratory test showed no relevant alterations (hemoglobin = 13.2, hematocrit = 42.2, leukocytes = 7.2, platelets = 336 000, glucose = 88, prothrombin time = 13, thromboplastin time = 27.8).
We intended to perform a conventional gastric sleeve [6], however, while dissecting the esophageal hiatus, a tumor-like mass was identified, which depended on the left lateral face of the distal third of the esophagus (Fig. 1). We decided to perform a pneumatic test and trans-surgical endoscopy to rule out any type of communication of the mass with the esophagus. Once the possible connection between the esophagus and the tumor mass has been discarded, the dissection continued, managing to remove the tumor mass which measured ~4 × 5 cm (Fig. 2) and it was sent to pathology for study (Figs 3 and 4). Finally, hiatus repair was performed and the gastric sleeve was completed in a conventional manner. A leak test was performed, confirming the integrity of the sleeve and the esophagus.
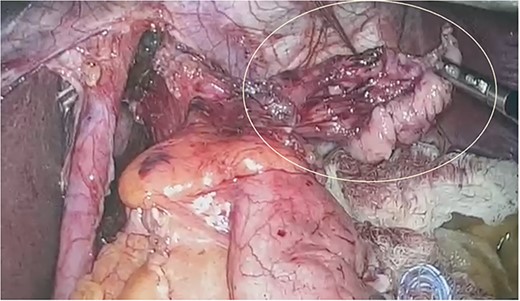
Tumor-like mass identified on the left lateral face of the distal third of the esophagus.

Macroscopic image of the tumor found, irregularly shaped tissue fragment measuring 4.3 × 2.9 × 2.1 cm.
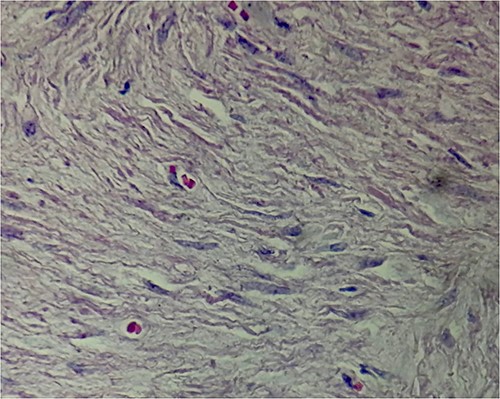
Fusiform hypercellular population in long and short bundles as well as hypercellular confluences with extensive myxoid edematous hypocellular areas.
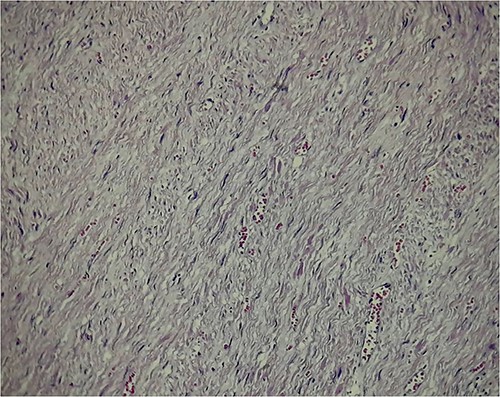
Abundant dilated congestive vascular structures; at higher magnification of spindle cells with pale acidophilic cytoplasm, elongated nuclei of vesicular chromatin, with smooth muscular characteristics.
The histopathological study did not report any abnormal mitotic activity and the tumor was classified as an esophageal leiomyoma.
In the post-operative period, the patient reported no abnormalities or discomfort, wandering at 8 hours and adequately tolerating the resumption of oral intake at 48 hours. A new leak test was performed, which revealed no abnormalities in the digestive tract, and she was discharged from hospital. One month after her surgery, the patient had a weight loss of 10 kg and was reported to be without complications.
DISCUSSION
Benign tumors of the esophagus are lesions that are rarely found; of these, the most frequent are leiomyomas, which constitute two-thirds of them, and the most frequent age of appearance is between 20 and 50 years of age [7]. Because leiomyomas do not normally present characteristic symptoms, they are usually found as a finding; they are benign mesenchymal tumors derived from the smooth muscle [5]. When it is a large tumor, it can be symptomatic, and the most common symptoms are bleeding (acute or chronic), abdominal pain, nausea, weight loss and dysphagia [8].
The discovery of these type of lesions in the trans-surgical can be frightening due to the malignant potential that they may have. However, it has been described that these kind of findings can be managed laparoscopically during the same surgery, and the decision to finish the procedure or not should not be taken lightly [9]. A pre-surgical endoscopy can be controversial, but in this case, doing the trans-surgical endoscopy gives us a tool to determine whether to continue the surgery or not. Based on this case and the experience of some studies, it is shown that when the surgeon is faced with an unexpected finding in the surgical procedure, it can be resolved by laparoscopy. In fact, due to the high risk that derives from general anesthesia and due to the benefits of bariatric surgery, the recommendation of some authors is to conclude the originally planned procedure once the tumor has been removed, as in this case, as long as the lesion can be delimited and has clear margins [10].
Some authors recommend performing a preoperative endoscopy in the evaluation of patients [10], however, this remains a controversial issue. Madan et al. recommend carrying out this practice because they found that treatment can often change according to the findings evidenced in the endoscopy [11]. Similarly, Sharaf et al. have the same recommendation as they described up to 120 patients (61.5%) with clinically important findings in preoperative endoscopy [12]. On the other hand, authors such as Peromaa-Haavisto et al. do not consider pre-surgical endoscopy to be necessary, because in their study, in addition to the fact that all their findings were benign and without clinical relevance, none of them modified the initial surgical plan [13].
Whether or not an endoscopy is decided to be performed during the preoperative evaluation of the patient, unexpected findings during surgery may continue to appear, so the surgeon and his team must always be prepared.
In conclusion, unexpected findings during surgery may occur from time to time, and they should be resolved during surgery when possible to allow the completion of the originally planned surgical procedure.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



