-
PDF
- Split View
-
Views
-
Cite
Cite
Nicholas B Capal, Steven A Neubauer, Sean C Reimer, Case report: bowel perforation after cutaneous nerve radiofrequency ablation for postherniorrhaphy neuralgia, Journal of Surgical Case Reports, Volume 2022, Issue 7, July 2022, rjab592, https://doi.org/10.1093/jscr/rjab592
Close - Share Icon Share
Abstract
Postoperative inguinal neuralgia is a known complication of open or laparoscopic herniorrhaphy, initially managed conservatively with analgesics. If symptoms do not resolve additional treatment modalities include nerve blocks, mesh explanation, neurectomy or radiofrequency ablation. Radiofrequency ablation is also used for ablation of hepatic tumors, and thermal injury to bowel is a known and well-documented complication with its use on the liver. There is no published literature or case reports describing thermal injury to bowel from radiofrequency ablation of ilioinguinal or iliohypogastric nerves. We present a case of a 44-year-old male with postoperative inguinal neuralgia following bilateral herniorrhaphies. He failed conservative management and underwent hot radiofrequency ablation of bilateral ilioinguinal and iliohypogastric nerves and presented with delayed small bowel perforation due to thermal injury.
INTRODUCTION
Chronic groin pain following inguinal hernia repair secondary to nerve injury or entrapment can be debilitating and severe. The ilioinguinal and iliohypogastric nerves are frequently implicated in chronic inguinal neuralgia following surgery [1]. If conservative treatment measures fail to relieve symptoms, additional treatment modalities may include nerve block, mesh excision, surgical neurectomy or radiofrequency (RF) ablation [1–4]. Hot RF ablation, which uses electrical current and frictional heating to cause tissue necrosis [5]. Hot RF ablation is safe and effective for treating postherniorrhaphy neuralgia [3, 4]. A feared complication with the use of hot RF ablation on hepatic tumors is bowel injury or perforation secondary to thermal injury [5–7]. Although bowel perforation has been well-documented with hot RF ablation of hepatic lesions, to our knowledge, there are no reported cases of thermal bowel injury and perforation following cutaneous nerve hot RF ablation. Here we describe a case of a bowel perforation from thermal injury following hot RF ablation of ilioinguinal and iliohypogastric nerves for postherniorrhaphy neuralgia.
CASE REPORT
A 44-year-old male presented with persistent abdominal pain 7 days after undergoing RF ablation of ilioinguinal and iliohypogastric nerves. The patient has a history of bilateral inguinal hernia repair with mesh, subsequently he was noted to have left-sided recurrence which was treated with open repair. The patient has had persistent complaints of pain following the hernia operations and was eventually referred to pain management for chronic postherniorrhaphy inguinal neuralgia.
He presented to the emergency room with worsening lower abdominal pain for 1 week after undergoing bilateral ilioinguinal and iliohypogastric hot RF ablation with Pain Management. Per outside hospital, he underwent RF ablation at 80°Cfor 90 s. Computed tomography imaging was obtained which showed an inflamed area of small bowel with a localized area of pneumoperitoneum (Fig. 1). Given his normal vitals, lack of peritoneal findings on abdominal exam, and leukocytosis 14 000 with otherwise unremarkable lab work, we elected to initially treat with IV antibiotics, bowel rest and serial abdominal exams. On hospital Day 3, he was taken to the operating room for persistent pain and failure to improve. A diagnostic laparoscopy was performed. There was a scarred area on the peritoneum with adherent small bowel and omentum found. This single adhesion was taken down and the involved jejunal segment was inspected revealing a full-thickness perforation with surrounding erythematous bowel (Fig. 2). The intraoperative findings and timing post-RF ablation were consistent with delayed perforation secondary to jejunal thermal injury. A laparoscopic small bowel resection with intracorporeal stapled anastomosis was performed. His postoperative course was uneventful, and he was ultimately discharged post-op Day 3 after tolerating a diet and having bowel function.
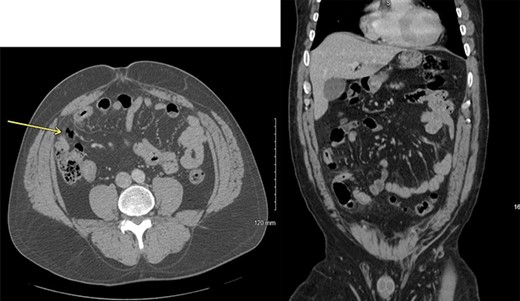
Axial and coronal computed tomography scan views of the patient showing small area of pneumoperitoneum with surrounding small bowel inflammatory changes.
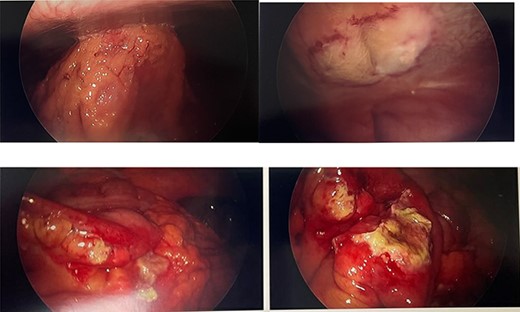
Intraoperative photos. Top right: omentum and small bowel adhered to anterior abdominal wall. Top left: scarred peritoneum after removing adhesion, lateral to medial umbilical ligament. Bottom: small bowel with isolated full-thickness necrosis and perforation and surrounding erythema from thermal injury.
DISCUSSION
Colonic perforation is a known complication associated with RF ablation of the liver [5–7]. Although colonic perforation following RF ablation of liver lesions is well-documented, there are no reported cases of thermal injury and bowel perforation following hot RF ablation of a cutaneous nerve.
Hot RF ablation uses electrical energy to cause frictional heating and coagulation necrosis of tissue [5, 7]. If bowel or other structures are in close proximity (within 1–1.5 cm) to the ablation target, then inadvertent thermal injury can occur during ablation of liver lesions [5, 7]. Increased risk of bowel injury was found in patients with history of prior cholecystectomy, bowel resection or any adhesive disease affixing the hepatic flexure of the colon to the liver [8]. In our case, the patient did have a history of lower abdominal surgery from previous inguinal hernia repairs, but no adhesions other than the single reactive adhesion at site of bowel injury were identified during laparoscopy. Adhesive disease placing the bowel in close proximity to the anterior abdominal wall to cause thermal damage was unlikely the cause. In this case, it is possible that the bowel was in close proximity to the area of ablation due to our patient’s nonobese body habitus (BMI 28). On cross-sectional imaging the distance of the small bowel to area of ablation is just over 1 cm, which could have resulted in inadvertent thermal injury.
Some techniques have been proposed to increase the distance between adjacent organs and target tissue during hot RF ablation of the liver in order to decrease the risk of inadvertent thermal damage. One technique involved instillation of water or 5% dextrose into the peritoneal cavity to displace bowel from target tissue in the liver [7]. A noninvasive technique described involves positioning the patient on the odds ratio table to use gravity to help shift bowel away from the ablation area [7]. In vascular surgery, both extreme Trendelenburg positioning and instillation of tumescent fluid circumferentially for saphenous vein RF ablation is used to increase the distance of adjacent deep veins to limit thermal spread and potential endothermal heat-induced thrombosis [9]. In hindsight, placing the patient in reverse Trendelenburg could have been beneficial to displace the small bowel cephalad and increase the distance from ablation and potentially prevent a thermal injury and additional morbidity for the patient.
In conclusion, thermal injury and bowel perforation is a complication following hot RF ablation of the liver. Although not described in the literature or case reports until now, thermal bowel injury can also occur following hot RF ablation of cutaneous nerves. The techniques used to decrease the proximity and risk of inadvertent thermal injury for hepatic or vascular RF ablation might have helped our patient’s case.
CONFLICT OF INTEREST STATEMENT
None declared.



