-
PDF
- Split View
-
Views
-
Cite
Cite
Foteini Karasavvidou, Lampros Mitrakas, Maria Strataki, Dimitrios Anastasiou, Georgios Koukoulis, Vassilios Tzortzis, Poorly differentiated muscle-invasive giant cell tumor of the bladder leads to unfavorable clinical outcome, Journal of Surgical Case Reports, Volume 2022, Issue 4, April 2022, rjac046, https://doi.org/10.1093/jscr/rjac046
Close - Share Icon Share
Abstract
Urothelial carcinoma of the urinary bladder is a common clinical entity. Recently, researchers focused on the emerging clinical significance of histologic variants, because they may need special therapy and their prognosis differs. Hereby, we describe a case of a giant cell osteoclast-like urothelial carcinoma of the urinary bladder.
INTRODUCTION
Urothelial carcinoma (UC) of the urinary bladder has a great propensity to undergo divergent differentiation. The resulting subtypes are morphologically unique and have significant prognostic and therapeutic differences. Osteoclastic-rich undifferentiated carcinoma (ORUC) of the urinary bladder is an extremely rare and aggressive variant of high-grade UC. The prognosis is poor. We describe the case of a 62-year-old man with a giant cell osteoclast-like UC of the bladder.
CASE PRESENTATION
A 62-year-old Caucasian male was referred from a private practice to the emergency department of our hospital, because of persistent macroscopic hematuria and hydronephrosis of the left kidney, due to a sizeable tumor of the urinary bladder. He was a smoker (~40 pack years), had no relative family history and no other comorbidities. Initial imaging with abdomen ultrasound showed an intraluminal bladder tumor (91×59mm) and a third-grade dilatation of the left pelvicalyceal system. Under antibiotic prophylaxis, transurethral resection (TUR) successfully controlled the hematuria. Moreover, a nephrostomy tube was placed on the left kidney. The histologic report documented a muscle-invasive (pT2) high-grade carcinoma with features of osteoclast-rich UC. After the TUR, detailed imaging (abdomen and thorax computed tomography, bone scintigraphy) showed cT3N0M0 disease. On this basis, a radical cystoprostatectomy and pelvic lymphadenectomy with a Bricker ileal conduit urinary diversion (RCPL-BUD) was performed. Histological examination revealed a pT4aN2M0 tumor with a biphasic appearance, with a mixture of mononuclear malignant epithelial cells and multinucleated osteoclast-like reactive giant cells. Mononuclear cells had abundant cytoplasm, round to oval vesicular nuclei and mild to moderate atypia. Mitotic figures were frequent (shown in Fig. 1). No finding of high-grade papillary or in situ UC was detected. Immunohistochemical examination revealed that the mononuclear malignant epithelial cells were positive for cytokeratins AE1/AE3, p63 and GATTA-3. The giant cells were positive for CD 68 (shown in Fig. 2). Subsequently, the patient was referred to the Oncology Department of our hospital for adjuvant cisplatin-based chemotherapy. The patient experienced recurrence and progression at about 7 and 11 months, respectively, after the RCPL-BUD. He died about 13 months after the original TUR diagnosis. This research complies with the guidelines for human studies and was conducted ethically in accordance with the World Medical Association Declaration of Helsinki.

Pathologic examination shows osteoclast-like giant cell carcinoma (H&E, ×100). Insert (H&E, ×400).
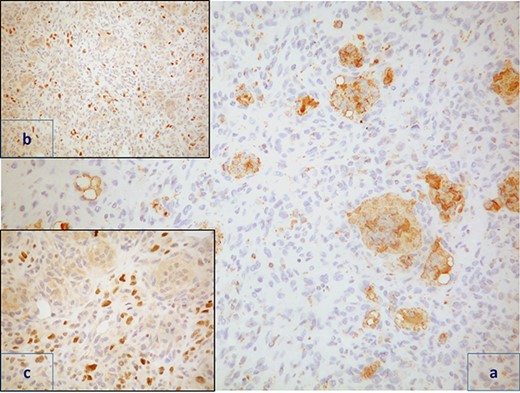
Immunohistochemical staining shows that the osteoclast-like giant cells were positive for CD68 (a, CD68 ×200). Mononuclear cells were positive for p63 (b, p63 ×100) and GATTA3 (c, GATTA3 ×20).
DISCUSSION
ORUC is a rare variant of UC. Less than 30 cases are reported in the literature. Histologically, it mimicks the giant cell tumor of bone (GCTB). The histogenesis is not clarified yet. Its urothelial origin is based on the positive reaction of an epithelial marker on mononuclear undifferentiated tumor cells and the existence of foci of ‘usual type’ UC component in some cases. In 1985, an urinary bladder tumor with giant cells that histologically mimicked GCTB was first reported by Kitazawa et al. [1] and was designated as ORUC of the urinary tract (UT) by Baydar et al. in 2006 [2]. According to the World Health Organization Classification of Urinary System Tumors (2016), it is a subset of ‘poorly differentiated tumors’. The most common locations in the UT are the kidneys, renal pelvis and bladder. Only two cases with ureter involvement are documented [3, 4]. They affect most frequently males in their seventh decade. There are no specific symptoms. Gross hematuria is most frequently observed.
ORUC of the UT closely recapitulates the morphology of osteoclastic GCTB or soft tissues. Histopathologically, the tumor has a biphasic appearance with a mixture of mononuclear malignant epithelial cells and multinucleated osteoclast-like reactive giant cells. Mononuclear cells have abundant cytoplasm, round to oval vesicular nuclei, mild to moderate atypia and variable mitotic activity. Severe pleomorphism is not usually seen. Mitotic figures are often frequent and atypical mitoses can be observed. The giant cells are morphologically and immunohistochemically identical to osteoclasts and are regarded as being of histiocytic origin. They are cytologically bland, may exhibit phagocytic activity but no mitotic activity and are uniformly distributed among mononuclear cells although they may condense around hemorrhagic foci. Prominent vascularity, large areas of hemorrhage, blood-filled cysts, red extravasation and deposition of hemosiderin, multinodular or sheet-like growth pattern and phagocytosis by giant cells are also common features with GCTB. In most cases, there is an associated high-grade papillary or in situ UC. Immunohistochemically, mononuclear cells are positive for cytokeratin, EMA, vimentin, Ki67, p53, GATA 3, thrombomodulin and p63 [5]. Giant cells are positive for CD68, alpha-1 antitrypsin, acid phosphatase, vimentin, CD51, CD54 and negative for cytokeratin, EMA, GATA 3, thrombomodulin, Ki67 and p53 [5]. The rarity of this neoplasm and its resemblance to other giant-cell rich processes may pose diagnostic difficulties. The differential diagnosis mainly includes pleomorphic giant cell carcinoma, foreign-body type giant cell reaction and the giant cell carcinoma that shows obvious malignant bizarre giant cells.
The terminology, histogenesis and biologic behavior of ORUC remain controversial. Their intimate association with UC along with their immunohistochemical profile supports an epithelial origin for mononuclear cells and a non-neoplastic reactive histiocytic lineage for osteoclast-like giant cells. Despite histological similarities, GCTB and ORUC of the UT have significantly different biological behaviors. GCTB are slow growing, locally aggressive and generally benign tumors. In contrast, the ORUC of the UT has an aggressive behavior and poor outcome. As seen in the literature, the patients died due to the disease in about 15 months. Our patient had a recurrence-free survival of about 8 months, a progression-free survival of about 12 months and a cancer-specific survival of approximately 13 months.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



