-
PDF
- Split View
-
Views
-
Cite
Cite
Inez Eiben, Darab Bahadori, Paola Eiben, PennyLouise Hever, Invasive cutaneous squamous cell carcinoma resulting in arm amputation. Case discussion and literature review, Journal of Surgical Case Reports, Volume 2021, Issue 12, December 2021, rjab534, https://doi.org/10.1093/jscr/rjab534
Close - Share Icon Share
Abstract
Skin cancer is one of the most common cancers in the world. Specifically incidence of non-melanoma malignancy in the UK has increased by 56% in the last decade. Cutaneous squamous cell carcinoma (cSCC) is a type of non-melanoma skin cancer that if caught early can be successfully treated. Conservative excision surgery is the most common treatment modality with high cure rates even if tumours are advanced. Radical surgery is rarely required, and amputations, especially when the distal part of the upper extremity is involved, are very uncommon. Here, we describe a case of an invasive cutaneous squamous cell carcinoma of the elbow that required trans-humeral arm amputation.
INTRODUCTION
Cutaneous squamous cell carcinoma (cSCC) is the second most common skin cancer. It arises due to abnormal proliferation of keratinising cells or appendages of epidermis [1]. It is a locally invasive cancer that can metastasise and despite attempts to improve knowledge about prevention its incidence is rising across the world.
It is most prevalent in Caucasians, males and elderly and anatomically on the head and neck, likely due to an increased exposure to ultraviolet radiation (UVR). Factors involved in etiopathogenesis include UVR exposure, Fitzpatrick skin types I and II, chemical carcinogens, immunodeficiency, chronic inflammation and pre-malignant conditions including Bowen’s disease, actinic keratosis and keratoacanthomas.
Phenotypic presentation usually consists of an indurated, keratinising, nodular tumour that can ulcerate. Depending on cSCC type, the course of the disease can be variable. Here we describe an unusual case of large, exophytic cSCC to the left elbow with deep local invasion, likely developed as a consequence of chronic tissue injury. To our knowledge, this is the first case to describe such a lesion.
CASE REPORT
An 82-year-old male was referred to the plastic surgery unit following request for a second opinion on an unhealing wound to the left elbow (Figs 1 and 2). For the past 20 years, he was suffering from left olecranon bursitis. Over the last 2 years, he developed a non-healing wound over the area needing managed with surgical washout and debridement. An investigation with magnetic resonance imaging (MRI) scan at the time showed simple collection over the left triceps muscle but no features of osteomyelitis or other pathology. Six months following debridement, there was still an area of non-healing sinus not improving with simple dressings.

Posterior view of the left elbow at initial presentation. Raised, ulcerated, keratotic tumour with surrounding chronic inflammatory change to the skin. A sinus in the centre of the wound is present. Width of the wound is 5 cm.

Posterolateral longitudinal view of the lesion at initial presentation. The proximal to distal dimension extends as far as 8 cm.
The patient was a right hand dominant ex-black cab driver with past medical history of hypertension, heart failure, chronic obstructive pulmonary disease and tissue aortic valve replacement. He was taking aspirin and was an ex-smoker. The examination revealed a 6 cm × 5 cm area of ulcerated, keratotic, chronic wound over the left olecranon with features suspicious of cSCC. No neurovascular deficit was discovered, and no other lesions were identified.
He was investigated with incisional biopsy of the lesion; four samples confirmed poorly differentiated cSCC. Further MRI imaging showed deep invasions of the cubital joint including, olecranon and ulna, and associated infiltration of the ulnar nerve and distal triceps (Figs 3 and 4). Positron emission tomography scan showed no distant metastases.
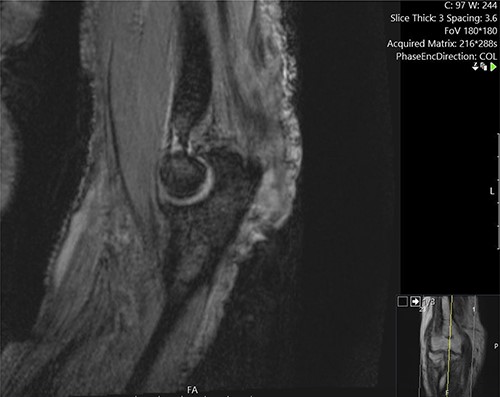
Sagittal MRI image demonstrating the invasion of the lesion into the, olecranon and distal triceps.
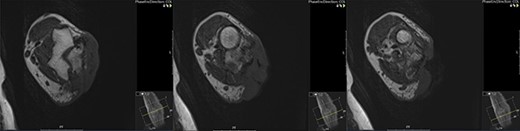
Cross-sectional MRI images demonstrating the position of the lesion and its infiltration into the joint space and deep tissues including the ulnar nerve.
Following a discussion at a plastic surgery and dermatology meeting, we concluded the need for trans-humeral amputation in favour of wide local excision and free flap reconstruction given patient comorbidities. The patient underwent the procedure as per the British Association of Dermatologists guidelines. Biopsies analysed following surgery showed no residual tumour demonstrating complete excision. No adjuvant therapy was required, and at 1 year post excision, the patient is fully recovered.
DISCUSSION
Common cSCCs, especially in the region of the head and neck, account for 80–90% of all tumours [2] and are usually indolent tumours. They show good prognosis with >90% 5-year survival rate when treated correctly and <4% metastatic rates [3]. The disease can be divided into common primary disease that depending on the recurrence rate is further stratified into low and high-risk tumours, and advanced disease. Advanced tumours are classified into locally advanced or metastatic and are likely the ultimate step of prolonged intraepidermal dysplasia from malignant proliferation of keratinocytes [4].Notably, advanced sCCs are often the result of a highly biologically aggressive type of tumour or multiple relapses due to incorrect management, similarly to the described case.
The aim of treatment is the clearance of the tumour. Additional objectives are the preservation of relative function and cosmesis. With effective treatment, most cSCCs have >90% cure rate [5]. In high-risk tumours, this requires invasive treatments and often radical surgery. However, given the often slow progression and extension, most tumours are diagnosed and treated before they show extreme locally invasive features. In this case, the delay in diagnosis could be the result of the chronicity of the wound the patient has been suffering from, or the delays associated with the COVID-19 pandemic.
Although cSCC in the presence of chronic inflammation is a rare but known phenomenon, as described in the cases of Marjolin’s ulcer [6], we were unable to find cases of inflammation-driven cSCC or extensive locally advanced disease to the arm in a PubMed search. Although a singular case presented inflammatory-driven cSCC to the forearm [7], the majority of described tumours involved the digits and the hand only. Furthermore, the data on management of invasive cSCCs of the trunk and the extremities is limited to retrospective studies and case studies. The importance of establishing the optimal standardized way of treatment cannot be overemphasised. Accordingly, in an attempt to design a management protocol, we extrapolated recommendations from head and neck cases. These indicated that multimodal management improves outcomes and that outcomes are largely dependent on the clinical setting [8]. When considering surgical management, literature suggests that the presence of clear margins following high-risk cSCC excision is associated with 95% local control and close to 99% disease-specific survival [9]. This is not accurate, however, when examining more invasive lesions like presented in this case. Specifically, local control numbers drop to 50–55% in cases of macroscopic perineural invasion. One of the reasons for this significant reduction may be that invasive cSCCs are not respecting anatomical tissue borders [8], which then leave no option but to treat the disease with radical surgery and limb amputation. Therefore, it is extremely important to aim to initiate treatment early and prevent extensive invasion, as limb amputation can lead to major complications and significantly affect patient’s quality of life. Though this is important to all skin cancers, it is especially relevant to cSCC as with early detection many amputations can be avoided. Different strategies have been tried to tackle this problem including education on sun exposure behaviours, which can be altered effectively by multicomponent tactics implemented from a young age [10]. Furthermore, chemopreventive agents like retinoids and non-steroidal anti-inflamatory drugs (NSAIDS), are currently being tested as potential agents that decrease the risk of developing new cSSCs in at-risk patients.



