-
PDF
- Split View
-
Views
-
Cite
Cite
Yohei Kawatani, Atsushi Oguri, Minimal incision superficialization of the brachial artery: a technical note, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa292, https://doi.org/10.1093/jscr/rjaa292
Close - Share Icon Share
Abstract
The Japanese Society for Dialysis Therapy recommends superficialization of the brachial artery (BA) for vascular access in patients with comorbidities. We describe a novel minimal incision superficialization surgery of a BA through a single small incision. A 78-year-old male, who underwent chronic hemodialysis through an arterio-venous fistula, was transferred to our hospital for treatment of heart failure. We chose superficialization of the right BA for new vascular access. Under tumescent local analgesia, though a single 2-cm long incision, the BA was superficialized for 10-cm long. To complete procedures in the narrow and deep space, vessel branches were ligated by vascular clip and knot-less barbed suture was applied for closure of the brachial fascia beneath the BA. The hemodynamic status during the hemodialysis improved and the New York Heat Association (NYHA) classification grade improved from IV to II. This technique can be an alternative for arterio-venous fistula in patients with comorbidities.
INTRODUCTION
The concept of superficialization of an artery for vascular access was introduced by Britter et al. in 1970 [1]. According to the guidelines of the Japanese Society of Dialysis Therapy, this technique is recommended for patients with comorbidities [2]. Although recommended in the guidelines, a standard method has not been established. Moreover, there are only a few reports on the use of a single small incisions to superficialize an artery.
CASE PRESENTATION
A 78-year-old man with a history of chronic hemodialysis through an arteriovenous fistula (AVF) was transferred with gradually progressing chronic heart failure (NYHA IV). Ultrasound cardiography revealed that the left ventricular ejection fraction was 36%, with an estimated pulmonary systolic pressure of 38 mmHg and a pressure gradient of 44 mmHg for the aortic valve. During hemodialysis, norepinephrine was administered at a rate of 0.03–0.06 μg/kg/min to maintain the systolic blood pressure >60 mmHg. The patient also suffered from ischemic steal syndrome associated with the AVF.
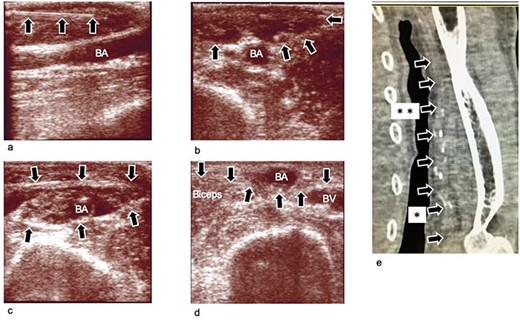
Ultrasound images obtained during and after the operation, (a) Ultrasound image obtained during infusion of TLA solution into subcutaneous tissue. The needle is clearly seen (arrow mark). (b) Ultrasound image obtained after infusion of the TLA solution into the subcutaneous tissue. The subcutaneous tissue becomes edematous (arrow mark). (c) Ultrasound image obtained after infusion of the TLA solution around the BA. The compartment becomes edematous. The BA is dissected from the fascia surrounding it. (d) Ultrasound image obtained 3 weeks after the operation. The BA is transposed to the subcutaneous layer, which is superficial to the brachial fascia (arrow). (e) Plane computed tomography image obtained 4 weeks postoperatively. The BA (arrow marks) is transposed to the subcutaneous layer. The transposed lesion was between arrow marks with * and **. The transposed length was 10 cm, and the depth of the lesion was 2 mm, which was just beneath the skin. BA: brachial artery; BV; brachial vein; TLA: tumescent local analgesia.
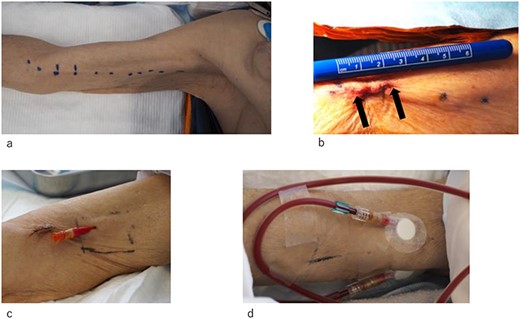
Photographs of the right upper arm obtained before and after the operation. (a and b) The position of the BA is marked on the skin. The operation is performed through a 2-cm incision. The incision is indicated by arrow mark. (c and d) The BA and cephalic vein are safely cannulated with a 16-gauge needle.
We performed a right brachial artery (BA) superficialization for creating a new vascular access as it was necessary to ligate the chronic AVF. First, a total of 42 ml of tumescent local analgesia (TLA) solution (430 ml of normal saline, 20 ml of sodium bicarbonate, 50 ml of 1% lidocaine and epinephrine at a concentration of 1 000 000:1) was injected into the subcutaneous tissue of the right upper arm and around the right BA under the brachial fascia (Fig. 1). A 2-cm skin incision was then created (Figs 2a, b and3a) 3 cm proximal to the cubital crease. The subcutaneous tissue and brachial fascia were subsequently divided along with the course of the BA using a 15-mm wide and 10-cm long retractor and forceps. This procedure created a subcutaneous tunnel to transpose the BA. Then, the BA was exposed (Fig. 2a and b). The BA was dissected from the fascia, the brachial veins and the median nerve using the same retractor and forceps. The branches of the BA were ligated using a vessel ligation clip (LIGACLIP, Ethicon, Inc., Cincinnati, USA) and divided. The brachial fascia was incised to transpose the BA, and the fascia was closed with a running suture using a 4-0 absorbable barbed suture (Stratafix spiral, Ethicon, Inc., Somerville, USA) beneath the BA. A total of 10 cm of the BA was transposed to subcutaneous plane (Fig. 3d, e and f) and superficialized (Fig. 1e). No drain was placed. We then, ligated and divided the AVF on the left forearm.
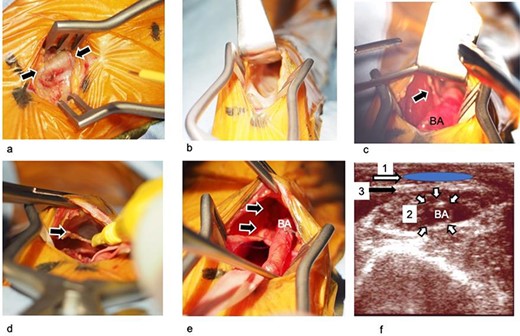
Photographs and schematic images of the operative method. (a) The BA is exposed through the incision. The surrounding tissue is edematous due to injection of the TLA solution but did not interfere with surgical procedures. (b) The subcutaneous tissue and brachial fascia are dissected using a retractor and a pair of forceps. (c) The BA is dissected from the surrounding tissue including the brachial fascia, brachial vein and brachial nerve. The branches are ligated with a ligation clip. Arrow mark; branches of the BA. (d) The brachial fascia is cut. Arrow mark; brachial fascia, which is being cut. (e) The brachial fascia is closed with barbed absorbable sutures beneath the BA. Arrow mark: suture line of the brachial fascia (f) Schematic overview of procedures performed using cross-section ultrasound imaging. First, the subcutaneous tissue was dissected, and a subcutaneous tunnel was created (area ‘1’). Second, the BA was dissected from the surrounding tissues. The branches of the artery are ligated and divided (area ‘2’). Third, the brachial fascia above the BA was cut (membrane ‘3’). Finally, the fascia beneath the BA was closed; the BA was transposed to the subcutaneous tunnel. BA: brachial artery; TLA: tumescent local analgesia.
We used the superficialized BA 3 weeks after the transposition surgery. The transposed BA and the right cephalic vein on the right upper arm were used for outflow and inflow, respectively. Using a 16-gauge needle (Fig. 2c and d), the procedures of puncture and hemostasis were completed without any complications. The blood flow during dialysis was 150–250 ml/min, which was sufficient for continuing hemodialysis. The dry weight was similar to that before the surgery. The hemodynamic status was stable, and the systolic blood pressure was >80 mmHg, with norepinephrine administered at a rate of 0–0.02 mg/kg/min. The NYHA grade improved from IV to II.
DISCUSSION
Previous studies on BA superficialization have reported creation of 10–15-cm long incisions and superficialization of the BA for similar lengths. In these reports, lipectomy was performed and skin flaps were created; the BA was placed beneath the skin flap and on the enclosed brachial fascia [3, 4]. The skin flap is naturally prone to necrosis and wound dehiscence. Our surgery requires a single small incision and the creation of a subcutaneous tunnel, instead of fashioning a skin flap. This enabled us to avoid consequent skin complications. There are several reports regarding the use of several minimal incisions or endoscopic surgery to superficialize the cephalic vein to make an AVF [5, 6]; however, there are only a few reports on the use of a single small incision to superficialize an artery.
Procedures in the narrow space, such as through a minimal incision and the skin tunnel, are difficult and particularly challenging. To overcome these difficulties, we customized the procedures, devices and anesthetic technique involved. First, we used a vascular ligation clip that is designed to be used in narrow spaces, for ligation of the branches of the BA and brachial veins. Adequate hemostasis was attained and the procedure was performed safely. We did not observe any complication associated with the implanted metal clip. Second, we used a knot-less barbed suture (Stratafix spiral, Ethicon). This suture has a loop at its end that makes it possible to start suturing without making knots. Moreover, the barbs on the suture surface provide secure fixation for the running suture [7, 8]. In surgeries of superficialization of the BA, the brachial fascia should be closed beneath the BA. The procedure was performed successfully with the suture. Third, we used TLA for anesthesia in this operation. The water-dissection effect of TLA helped us in creating the subcutaneous tunnel and in exposing the BA. The administration of epinephrine resulted in vasoconstriction that made hemostasis easier and we encountered minimal bleeding during the procedure. One consideration for the use of TLA in this operation was the risk of ischemia because of the vasoconstriction of BA brought on by the epinephrine. In a report on the association of epinephrine in the analgesic solution and tissue ischemia in hand surgeries, a concentration of 100 000:1 epinephrine did not cause ischemic complications of the digital arteries and the authors concluded that the technique was safe [9]. In our surgery, the concerned artery was much larger in caliber than the digital arteries and the epinephrine was much more diluted at 1 000 000:1. We assumed our technique was safe. Our surgery did not require drain placement because of minor bleeding and exudate fluid.
To prevent complications associated with superficialized BA in the daily HD, enough length of superficialized artery is essential. Brachial artery superficialization for a length of 10–15 cm is reported to have good long-term patency [3, 4]. Sashi et al. [10] reported that the minimum straight segment required for an AVF is 10 cm. We also assumed that a length of 10 cm for superficialization was necessary in our procedure. We used the same criterion for the size of the BA and inflow veins as that used in conventional long-incision superficialization surgeries, that is, the size of the vessels are adequate if they can be cannulated by 16-gauge needles.
In conclusion, minimal incision superficialization of a BA performed successfully.
ACKNOWLEDGEMENTS
The authors are grateful to Naoki Kameyama and Shinya Watanabe for their help and support in the patient care and data analysis.
CONFLICT OF INTEREST STATEMENT
There is no conflict of interest.
FUNDING
None.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the local ethical committee (Approval number; thh 01-011). The consent to participate was obtained from the patient. The consent for publication was obtained from the patient.



