-
PDF
- Split View
-
Views
-
Cite
Cite
Akinobu Furutani, Sachiko Yoshida, Toshihiko Yoshida, Masayasu Nishi, Takashi Yamagishi, Hironobu Goto, Dai Otsubo, Hisoka Yamane, Taku Matsumoto, Yasuhiro Fujino, Masahiro Tominaga, A case of laparoscopic anterior resection for rectal cancer with duplication of the inferior vena cava using preoperative 3D computed tomography angiography, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa223, https://doi.org/10.1093/jscr/rjaa223
Close - Share Icon Share
Abstract
We report the case of a patient with duplication of the inferior vena cava (DIVC) who underwent anterior laparoscopic resection for rectal cancer. A 66-year-old woman presented with abnormal lung shadows on a chest x-ray during a routine health checkup. She was diagnosed with rectal cancer and lung metastasis using colonoscopy and thoracoabdominal computed tomography (CT). In addition, a 3D CT angiography revealed double inferior vena cava, one on either side of the aorta. The preoperative diagnosis was rectal cancer cT3N0M1a(Lung) cStage IVA with DIVC, and a two-stage surgery was planned. The first stage was high anterior laparoscopic resection. This was safely performed because the pre-hypogastric nerve fascia was preserved and the left inferior vena cava was not visualized during the surgery. During the second stage of the surgery, video-assisted thoracoscopic left lower lobectomy was performed and no recurrence was observed for >6 months after the second surgery.
INTRODUCTION
Duplication of the inferior vena cava (DIVC) is a rare congenital anomaly, and the incidence of DIVC is 0.2–3.0% of the general population[1]. The inferior vena cava (IVC) runs on both sides of the abdominal aorta; hence, due caution is necessary when mobilizing the sigmoid mesocolon during the surgery for rectal cancer. Laparoscopic surgery for the treatment of malignant gastrointestinal tumors in patients with DIVC is relatively rare. There are no published reports on laparoscopic surgery for colorectal cancer, in patients with DIVC. We report here, the case of a patient with DIVC who underwent anterior laparoscopic resection for rectal cancer.
CASE REPORT
A 66-year-old woman presented with abnormal lung shadows on a chest x-ray at a health checkup. She was diagnosed with rectal cancer and lung metastasis by colonoscopy and thoracoabdominal computed tomography (CT) at a different hospital and was referred to our hospital for surgery. Her medical history included total hysterectomy for a uterine fibroid. She had no significant family history of any illness. The serum carcinoembryonic antigen level had increased to 5.5 ng/ml, whereas the serum carbohydrate antigen 19–9 level was within normal limits (3.7 U/ml). Other laboratory results were unremarkable. Colonoscopy revealed a type 2 tumor localized in the rectosigmoid colon. An endoscopic biopsy revealed a well-differentiated adenocarcinoma. Contrast-enhanced CT showed a thickened rectal wall and a mass measuring 40 mm in diameter in segment 6 of the left lung. In addition, 3D CT angiography revealed double IVC, one on either side of the aorta. The left IVC was formed by the merger of the bilateral internal iliac and the left external iliac veins, which then merged with the left renal vein, and flowed into the right IVC (Fig. 1). Based on these findings, the preoperative diagnosis was rectal cancer cT3N0M1a(Lung) cStage IVA according to the 8th edition of the International Union Against Cancer TNM system along with DIVC, and a two-stage surgery was planned.
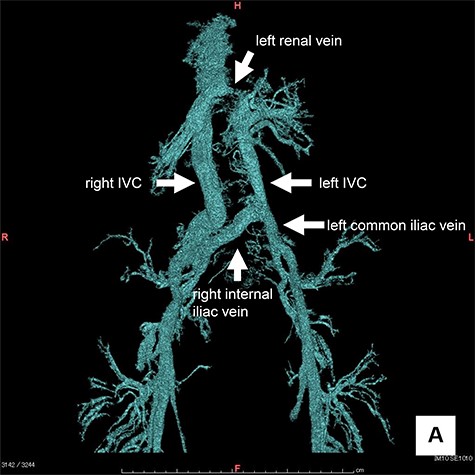
3D CT angiography: The left IVC was formed by the merger of the bilateral internal iliac and the left external iliac veins, which then merged with the left renal vein, and flowed into the right IVC.
The first stage of the surgery was high anterior laparoscopic resection with a five-port conventional technique, in which the sigmoid colon and upper rectum were mobilized via a medial approach. During the surgery, the left ureter, left gonadal vessels and hypogastric nerve plexus were identified and preserved. The left IVC was not visualized because the pre-hypogastric nerve fascia was preserved (Fig. 2). Hence, the surgery was performed safely. D3 lymph node resection was performed in accordance with the Japanese Society for Cancer of the Colon and Rectum Guidelines 2019 [2]. The duration of surgery was 259 min and blood loss was 10 ml. Her postoperative course was unremarkable, and she was discharged on postoperative Day 9. A surgical specimen showed type 2 tumor (27 × 49 mm) in the rectum and a pathological examination revealed a subserosal, invasive, moderately differentiated adenocarcinoma with metastasis in one lymph node. During the second stage of the surgery, video-assisted thoracoscopic left lower lobectomy was performed. Pathological examination of the left lower lobe tumor revealed a moderately differentiated adenocarcinoma, which was positive for cytokeratin 20 and negative for cytokeratin 7 immunohistochemical staining, indicating metastasis of the colorectal cancer. Finally, the tumor was diagnosed as pT3N1aM1a, pStage IVA according to the eighth edition of the International Union Against Cancer TNM system. No recurrence was observed for >6 months after the second surgery.
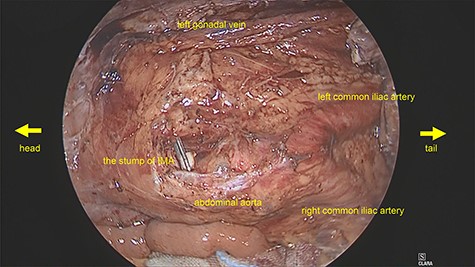
Intraoperative image: The left IVC was not visualized because the pre-hypogastric nerve fascia was preserved.
DISCUSSION
DIVC is a rare venous anomaly with an incidence of 0.5–3% [3]. The IVC develops from the subcardinal, supracardinal and posterior cardinal veins. Both posterior cardinal veins fuse to form the iliac veins and their confluence. The right supracardinal vein develops into the infrarenal IVC, and the left supracardinal vein regresses normally [4]. The right subcardinal-supracardinal anastomosis develops into the renal part of the IVC, and the right subcardinal veins along with the hepatic vein develop into the rest of the IVC [4]. Failure of regression of the left supracardinal vein leads to duplication of the IVC [4]. Almost all vascular anomalies are incidentally detected by CT or magnetic resonance imaging, and congenital anomalies of the IVC are commonly seen in asymptomatic patients as well.
In a typical anterior resection for rectal cancer, pre-hypogastric nerve fascia is preserved during mobilization of the mesosigmoid. The IVC, left ureter and left gonadal vessels are located behind the fascia, therefore, DIVC is not visualized during the surgery. In our case, the pre-hypogastric nerve fascia was preserved, and the surgery was performed safely. Currently, most resections for colorectal cancer are performed laparoscopically, and laparoscopic resection for rectal cancer with DIVC is an acceptable method. If resection of the para-aortic or lateral lymph nodes is planned for advanced colorectal cancer, it is necessary to be cautious about the abdominal aorta, IVC and iliac vessels during the surgery. Three-dimensional CT angiography is useful to understand the exact location of these vessels and the peripheral tissues. In our case, 3D CT showed that the left IVC was formed by the merger of the bilateral internal iliac and the left external iliac veins.
There are no reports of colorectal cancer with DIVC in English literature. In Japan, Mizuno [5] reported five cases of colorectal cancer with DIVC, and our case is the first report of laparoscopic resection for this condition.
CONCLUSIONS
This was a rare case of rectal cancer with DIVC, for which anterior laparoscopic resection was performed. If the pre-hypogastric nerve fascia is preserved, the anterior resection can be safely performed. 3D CT angiography is useful to understand the exact location of the DIVC and the iliac vessels.
ACKNOWLEDGMENTS
We would like to thank Editage (http://www.editage.jp) for English language editing.
References
- aorta
- computed tomography
- lung
- colonoscopy
- health evaluation
- laparoscopy
- neurons
- preoperative care
- chest x-ray
- surgical procedures, operative
- thoracoscopy
- inferior vena cava
- diagnosis
- fascia
- surgery specialty
- metastasis to the lung
- rectal carcinoma
- computed tomographic angiography
- left lower lung lobectomy



