-
PDF
- Split View
-
Views
-
Cite
Cite
Anh Binh Ho, Ngoc Son Nguyen, Vu Huynh Le, Duc Dung Nguyen, Anh Khoa Phan, Thanh Xuan Nguyen, Nhu Hiep Pham, Preoperative embolization of high-flow peripheral AVMs using plug and push technique with low-density NBCA/Lipiodol, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa316, https://doi.org/10.1093/jscr/rjaa316
Close - Share Icon Share
Abstract
Arteriovenous malformations (AVMs) embolization is considered as a promising option either its single treatment or in combination with surgery, and the use of low-density N-butyl cyanoacrylate (NBCA)/Lipiodol is acceptable mixture agents but its application should be performed by experienced endovascular teams. We describe a successful case preoperative embolization of high-flow AVMs with low-density NBCA/Lipiodol. A 26-year-old male patient was hospitalized with a big pulsatile mass at the right thigh. Doppler ultrasound showed a mass with high systolic, and diastolic velocities coming from the right superficial femoral artery. Angiogram showed a large and high-flow AVM type IV, according to Yakes classification. Low-density NBCA/Lipiodol 12.5% were performed to obstruct all the nidus and feeding arteries. Extirpation surgery was implemented 4 days after the complete embolization procedure.
INTRODUCTION
There are many subtypes of the arteriovenous malformations (AVMs). They are also called fistula and likely a messy shape of blood vessels [1]. The fully developed AVMs may produce symptoms gently as discomfort or more severely as ulcer with secondary infection. Fast-paced technological innovation is the key driving forces for the advent of endovascular embolization which is truly one of a good selection with minimally invasive treatment. The main goal is to give the patients a chance to avoid unnecessary resection, even if they need to have a surgery after intervention, it may reduce the risk of intraoperative bleeding [2]. Nowadays, N-butyl cyanoacrylate (NBCA) is allowable for some location-specific subtypes including muscoloskeletal AVMs. NBCA and Lipiodol are mixed together in a certain ratio which can visualize the vessel clearly and impale its polymerization time. The manipulation of NBCA should be expected to perform well by a reasonably interventional team [3]. Herein, we delightedly write up one preoperative embolization case of high-flow low-extremity AVMs.
CASE PRESENTATION
A 26-year-old male patient was hospitalized with a big pulsatile
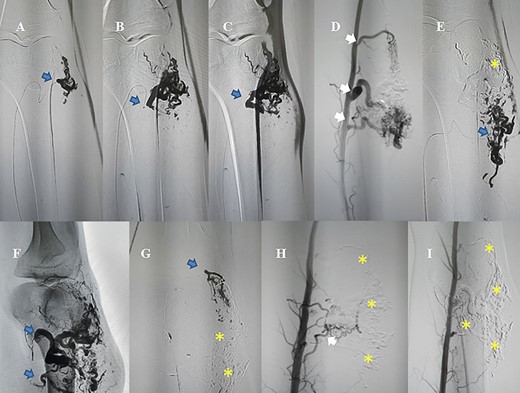
AVM embolization was performed through antegradely femoral approach; white arrows: the existence of feeding arteries need to be occluded; blue arrows: nidus and feeding arteries are being occluded by NBCA/Lipiodol; (asterisk) nidus and feeding arteries were totally occluded.
mass at the right thigh above the knee. The patient’s medical history is unclear about the previous injury. He felt discomfort and his physical examination revealed a pulsatile, palpable thrill mass. Doppler ultrasound showed a mass with high systolic and diastolic velocities coming from the right superficial femoral artery (SFA). Angiogram showed a large and high-flow AVM type IV coming from right SFA with three main feeding arteries, according to Yakes classification. A multidisciplinary discussion was required between surgeons and interventionists that ended with the conclusion of a preoperative embolization because of the high risk of intraoperative hemorrhage.
Firstly, antegrade approach at the right femoral artery was chosen with 45 cm—6 Fr—J tip guiding sheath. A microcatheter was manipulated into guiding sheath and the tip position was adjusted very close to the nidus. The guiding sheath was translated into the ostial of feeding arteries. Guiding catheter’s appearance in the ostial of the feeding branches is to reduce the distal low-limb occlusion due to liquid embolic agents when retrieving the microcatheter. Lower concentration NBCA/Lipiodol 12.5% (the ratio of the concentration is between 0.5 ml/0.5 mg NBCA and 3.5 ml Lipiodol) was aggregated. Plug and push technique was performed for injection under glue roadmap mode. Remarkably, when seeing the reflux stream very close to the tip of microcatheter which may have a risk of spreading to some normal branches of feeding artery or spreading out of the proximal part of feeding artery, the injection should be stopped and repeated 1 to 2 min later for glue concretion. When the reflux was seen at the ostial part of feeding artery, we stopped pushing NBCA/Lipiodol, pulled the microcatheter out and flushed the microcatheter with saline in preparation for another catheterization. In the case of microcatheter occlusion with unsuccessful flushing, new microcatheter will be used. These manipulations will be repeated until we positively see the disappearance of the contrast flow through the AVMs (parent vessel and nidus) under fluoroscopy.
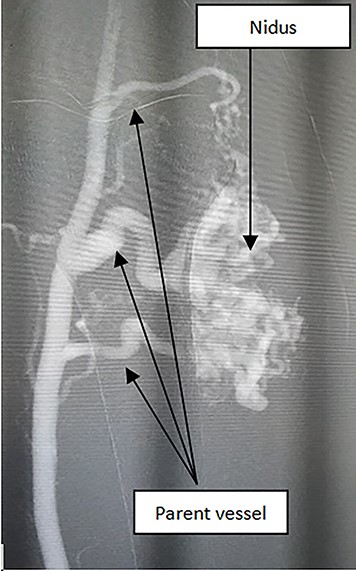
In the beginning, we recognized that this AVM has 3–4 main parent arteries (Fig. 1).
The patient had undergone an embolization (Fig. 2) and a surgical excision after 4 days (Fig. 3). The mean volume of injected NBCA/Lipiodol 12.5% was 15-20 mL. Clinical symptoms were medium pain and swelling. These symptoms decrease gradually and disappear within 4 days. No long-term peripheral circulation or pulmonary deficit was noted during the period of follow-up.

DISCUSSION
In our report, we examined the type IV AVM according to Yakes classification. Yakes developed a new classification of these lesions [4, 5]. NBCA was widely used because of these benefits, and the patient could accept it easier for a low-cost price, especially in a developing country.
NBCA is an acceptable agent currently available for AVMs embolization. The accuracy and safety of the embolization technique with NBCA is quite low because of unpredictable phenomenons such as reflux, migration, or immediate polymerization and thus some complications might be happened like off-target embolization and/or catheter gluing [6, 7]. To minimize complications, some researchers suggested low-dose density NBCA [8].
In our report, we diluted 0.5 ml/0.5 mg NBCA with 3.5 ml Lipiodol at the ratio 1:7, respectively, to have lower concentration (12.5%).
After embolization, the patient felt pain and burning sensation on the skin. These symptoms might come into contact with an allergen or an irritant, but they gradually decreased after a few days.
In conclusion, transcatheter embolization with diluted NBCA/Lipiodol is an acceptable treatment option at stopping hemorrhaging, especially in high-flow AVMs followed or not by surgical excision. Interventionists should have a good knowledge of the indications and complications and experience technique associated with NBCA use before practicing in a clinical situation.
Conflict of interest statement. The authors have no financial disclosures.



