-
PDF
- Split View
-
Views
-
Cite
Cite
Alex Guachilema Ribadeneira, Ángel Raúl Tapia Monard, Maria Cristina Endara, Cristian German Garcia, Milton Omar Sandoval, David Alejandro Cárdenas, Andrea Daniela Basantes, Intra-abdominal cystic lymphangioma of the mesocolon sigmoids: a rare entity in adult patient woman, Journal of Surgical Case Reports, Volume 2020, Issue 5, May 2020, rjaa031, https://doi.org/10.1093/jscr/rjaa031
Close - Share Icon Share
Abstract
The lymphangioma is a benign neoplasm, mostly connate, it occurs more often in children. It is more frequently located in the head–neck region, as well as in the armpit, and less frequently in the abdomen. The diagnosis, as well as their appearance is variant, they can be asymptomatic depending on the size. The signs on the physical exam are usually nonspecific and can look like an acute abdomen. Imaging tests used are the ultrasound and tomography, which determine the therapeutic behavior. The differential diagnosis should be made with other intra-abdominal injuries, such as cavernous hemangioma, mesotheliomas, pancreatic and ovarian tumors and even peritoneal hydatid cyst. The definitive treatment is surgical in most cases, with complete excision of the mass. The definitive diagnosis is obtained with the histopathological study of the surgical piece.
INTRODUCTION
Cystic lymphangioma of the mesentery is a rare intra-abdominal mass of uncertain etiology that constitutes 1/100 000 admissions in an adult hospital and 1/20 000 in centers for children [1]. More frequently in men than in women with a 1.5–3:1 ratio.
The clinical behavior of simple lymphatic and mesothelial cysts is usually asymptomatic and stable for years while lymphangiomas and benign mesotheliomas may be more aggressive and invasive, lack specific symptoms and patients are often admitted for complications.
We present the case of a cystic lymphangioma of the sigmoid mesocolon to whom complete mass excision was performed without any complications.
PRESENTATION OF THE CLINICAL CASE
Patient woman of 60 years of age, comes to our referred center of another health care center with a clinical picture of 5 years of evolution of abdominal pain, sporadic, located on the left flank and radiates to the lumbar region, accompanied by nausea and occasional vomiting. On the physical examination, we found a distended abdomen, painful on palpation on the left flank and hypogastrium, hard mass, immovable at the level of the left flank, is palpated.
Laboratory exams including blood count, glucose, urea, creatinine, coagulation profile, CEA and CA125 were within normal ranges.
The abdominal ultrasound performed reports, moderate fatty infiltrate to a predominance of the right lobe and a cystic aspect on the anechoic left flank.
Simple and contrasted tomography reports intraperitoneal oval occupational image at the left flank level of the abdominal cavity suggestive of mesenteric cyst.
Surgical procedure: laparotomy with supra and infra umbilical incision is performed, evidencing; cystic mass of ~15 cm in diameter translucent, dependent on the mesentery of the sigmoid colon attached but not infiltrated to the serosa (Fig. 1A).
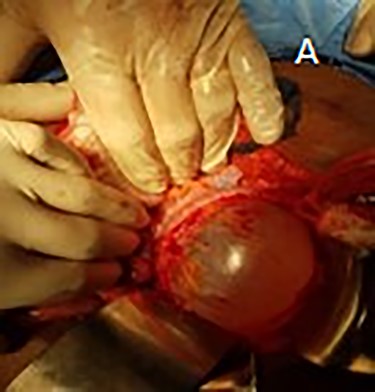
(A) presence of cystic mass located in the sigmoid colon mesentery.
We performed a Mattox maneuver with cystic mass exposure followed by meticulous dissection without devascularization of the affected colon segment (Fig. 2A–C).

(A) Exposure of cystic mass after Mattox maneuver. (B) Blunt dissection without mesocolon devascularization. (C) Surgical piece completely resected.
Favorable postsurgical evolution enters the surgery room in the postoperative period, a diet was started the next day, and it was discharged on the third day without complications.
The histopathological report: cystic mass of 11 × 8.2 × 7.6 cm in diameter and clear liquid inside. Microscopic: cyst wall lined by epithelium in two layers that sits on connective tissue and presence of eosinophils in the channels. PAS-AB refused to produce mucin, confirming a diagnosis of cystic lymphangioma.
DISCUSSION
The lymphangiomas are rare congenital malformations of the lymphatics characterized by the proliferation of the endothelium of lymphatic spaces [1,2].
Described for the first time by an anatomist in Florence in 1507 and officially described as cystic lymphangioma by Rockitansk. The first resection was performed by Tillaux in 1880 [1].
They can be located anywhere in the body, more commonly found in the head–neck region (75%) axillary region (20%) and less frequently in the mediastinum, retroperitoneum, mesentery, omentum, pelvis, groin, bone, skin, scrotum and spleen but very rare in the mesocolon (less than 1% of cases). In the abdomen, lymphangioma occurs most frequently in the mesentery, followed by the omentum, mesocolon and retroperitoneum [1–3, 5].
The exact prevalence of this condition is unclear, but it has been suggested in the literature that there are only 820 cases since the 16th century [4].
The incidence of lymphangioma of the mesentery is ~5%, and the male–female ratio is ~1.5–3:1 [2].
They are divided into three main types according to their histological characteristics: capillaries, cavernous and cystic. The first two types are seen as skin lesions, while the cystic type presents intra-abdominal or retroperitoneal [1].
With electron microscopy, two types of cells in them have been identified: endothelial and mesothelial. Based on this, they are divided into two groups: those of vascular origin (simple lymphatic cyst and lymphangioma) and those of mesothelial origin (simple mesothelial cyst, benign cystic mesothelioma and malignant cystic mesothelioma) [1].
Symptoms include abdominal distention are unspecific progressive and chronic pain when the tumor is large, you can compress the space, entrails or block the intestine, producing the corresponding symptoms.
Three forms of clinical presentation have basically been established:
Incidental finding;
Chronic or recurrent picture of abdominal pain and
Acute abdomen syndrome secondary to complications (intracystic hemorrhage, cyst infection rupture, intestinal obstruction and compression of mesenteric vessels).
The differential diagnosis is broad and should be made with other primary mesenteric tumors, metastatic disease, tuberculosis, pseudocysts, cystic teratomas, enteric duplication cysts and ovarian cysts [4, 6].
Laboratory data are not useful and what is requested is used to rule out malignant behavior of another etiology.
Ultrasound itself can be used to detect the location, size, division of the cyst, cyst fluid, cystic wall and its relationship with surrounding tissues. The diagnostic protocol is completed with an abdominal tomography that is more sensitive, it helps to differentiate from other entities and also serves for the decision and surgical approach [2].
The definitive treatment is the complete excision of the cystic mass and in many cases with resection of the anatomical structure affected. With complete excision, the results are excellent. However, incomplete excision has a high risk of recurrence [3].
Losanoff proposed a pathological classification considering the presentation of the cyst, as well as the possible resection: type I, pedicle; type II, sessile (both limited to the mesentery and these can be resected); type III, with retroperitoneal extension and type IV, multicenter, which may be impossible to dry out completely and in this case the surgery is palliative [7].
Percutaneous aspiration of the cyst is not recommended as a definitive treatment option but, it can be used for decompression followed by complete excision of the mass.
The pathological examination is the standard Gold, which gives the definitive diagnosis describing a thin wall with cystic wall lining of epithelial cells and a small amount of muscle tissue that can be seen. In addition, dilated and thin lymphatics can be observed.
The fact that the tumor depends on the sigmoid mesocolon and female patient gives a remarkable level of rarity in this case.



