-
PDF
- Split View
-
Views
-
Cite
Cite
Miguel Almeida, Luís Amaral, Duarte Viveiros, Victor Carneiro, Carlos Sebastião, Armando Medeiros, Paraduodenal mass as initial presentation of burned-out testicular tumour: case report and literature review, Journal of Surgical Case Reports, Volume 2020, Issue 3, March 2020, rjaa006, https://doi.org/10.1093/jscr/rjaa006
Close - Share Icon Share
Abstract
Testicular germ cell tumours (TGCTs) are relatively rare overall and are mainly encountered in young adults and teenagers. The ‘burned-out’ phenomenon refers to the spontaneous regression of the primary testicular lesion, generally with the presence of a metastatic germ cell tumour. Regressed tumours with retroperitoneal metastasis, as the first manifestation, represent difficult cases prone to misdiagnosis. Burned-out TGCT is a rare but well-recognized entity, with defined clinical features and diagnostic criteria; however, its etiopathogenesis is still not well defined.
We present a case of 37-year-old man with a retroperitoneal mass adjacent to the duodenum identified on CT scan. After surgical excision, histopathologic findings evidenced metastatic non-seminomatous GCT. Testicular examination was normal, but a right testis suspicious lesion was found on ultrasound study. Radical right orchidectomy was performed, and histological examination showed complete regression of TGCT. He underwent first-line chemotherapy with complete response and no evidence of recurrence.
INTRODUCTION
Testicular carcinoma represents only 1% of all neoplasm in men; however, testicular germ cell tumours (TGCTs), which account for over 90% of them, are the most common in young men (third and fourth decades), with increasing incidence. TGCTs are divided in to two histological groups: seminomas and non-seminomas, which include embryonal cell carcinoma, teratoma, yolk sac tumour, choriocarcinoma and mixed tumours [1, 2].
The term burned-out tumour describes a rare phenomenon in which the primary TGCT regresses, partially or completely, without any treatment. These tumours usually present as metastatic disease on the retroperitoneum, mediastinum, lymph nodes or other sites. Clinical manifestations generally depend on the metastatic disease, as the testicular clinical examination is often normal, leading to misdiagnosis [3].
Scrotal ultrasonography and serum tumour markers are useful, but histopathologic study with scar in the testicular parenchyma, with or without vestiges of GCT, is essential to the diagnosis of a regressed tumour. The etiopathogenesis of the regression is not well defined, and it is thought that less than 5% of all TGCTs undergo spontaneous regression [3, 4].
Chemotherapeutic strategies implemented in the 1970s for the treatment of advanced-stage TGCTs represent a paradigm shift to a curable disease [1, 5].
CASE PRESENTATION
A 37-year-old male patient, married with one child, without relevant past medical history, presented to emergency department with increasing upper abdominal pain, nausea and early satiety over the previous 2 weeks. On physical examination with pain and tenderness in the right upper abdomen, without other abnormal findings, specifically on the testicular examination.
Laboratory analysis revealed leucocytosis with neutrophilia and elevated C-reactive protein. Chest X-ray was normal. In the abdominal ultrasound, a 75 × 50-mm mass in topography adjacent to the duodenum was diagnosed. Abdominal CT scan displayed a complex retroperitoneal mass, predominantly cystic, adjacent to the duodenal third portion, with local inflammatory signs, without adenomegalies or other abnormalities (Fig. 1).

The patient was admitted for conservative treatment and further diagnostic investigation. The gastroduodenoscopy study showed a bulging in the third section of the duodenum mucosa with nodularity and congestion. Biopsy was unspecific. In the endoscopic ultrasound, the lesion limits were regular and well defined, however, with no cleavage plane with duodenal wall. Biopsies with insufficient specimen. Tumour markers: carcinoembryonic antigen 5.3 U/mL and carbohydrate antigen 19.9 (CA-19.9) 49.7 U/mL.
The patient was admitted for elective laparotomy with resection of the retroperitoneal mass en bloc with wedge duodenotomy and feeding jejunostomy. Histologic examination revealed neoplastic proliferation, with infiltration of the duodenum mucosa, consistent with retroperitoneal GCT metastasis, predominantly choriocarcinoma with immature teratoma foci (Fig. 2).
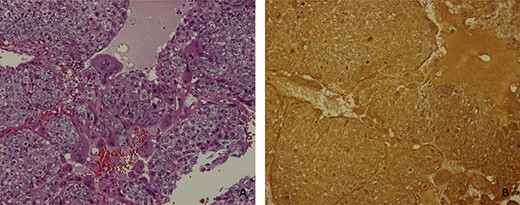
(A) mononucleated trophoblast cells and multinucleated synciciotrophoblasts with a haemorrhagic focus (H&E 10×); (B) β-hCG immunoexpression in neoplastic cells (H&E 10×).
After this diagnosis, the patient was re-evaluated, maintaining a normal testicular examination; tumour markers where rechecked: β-hCG 243 U/L, α-fetoprotein (AFP) 2.06 ng/mL and lactate dehydrogenase (LDH) was normal; sonography identified right testicle heterogeneity with a nodular hypoechoic area with internal calcifications (Fig. 3) and thoracic CT showed no relevant abnormality.
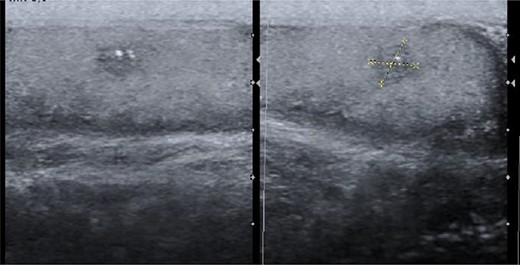
Scrotal ultrasound with a heterogeneous nodule with microcalcifications.
The patient was admitted for a radical right orchidectomy. Gross examination revealed a 5 × 4-mm, well-demarcated solitary, whitish scar, with focus of mononucleated inflammatory cells, siderophages, hyalinized tubules and increased vascularity on light microscope. At scar periphery, there was a germ cell neoplasia in situ (Fig. 4).
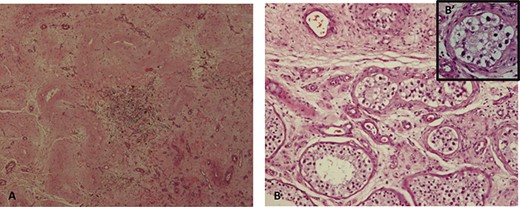
(A) fibrous scar with focus of lymphoplasmacytic inflammatory cells and hyalinized ghost seminiferous tubules; (B) sclerotic and atrophic seminiferous tubules peripheral to the scar (H&E 10×), (B′) some with germ cell neoplasia in situ (H&E 40×).
Subsequently, the patient underwent first-line chemotherapy with four cycles of bleomycin, etoposide and cisplatin (BEP) protocol. After the adjuvant treatment, the serum tumour markers (LDH, AFP and β-hCG) were normal, and in imaging evaluation, there is no evidence of recurrence.
DISCUSSION
TGCTs possess a considerable histological heterogeneity. Non-seminomatous GCT represent almost half of them, with peak incidence on the third decade. About, 50% have metastatic disease at presentation. Historically, choriocarcinoma has been considered the most prone to regression, but recent reports confirm that seminoma is the most common histology [1–4, 6, 7]. An exact incidence of burned-out tumours cannot be specified, although it is documented in approximately 10% of the patients who died of metastatic TGCT [7].
The TGCT burned-out phenomenon was first described by Prym et al. in 1927, and few decades later, the concept was refined by Azzopardi et al. in 1961. The spontaneous regression of the primary tumour has been described in different pathologies such as melanoma, lymphoma, renal carcinoma, among others. Although the mechanism behind regression has not been determined, there are two main hypotheses: the immunological theory of regression, involving an immunological response mediated by cytotoxic T lymphocytes that recognize tumour antigens and destroy malignant neoplastic cells, with subsequent fibrosis replacement; the other hypothesis is an ischemic response in the neoplasia, secondary to the blood supply deficit due to high metabolic rates and/or intermittent testicular torsion [3, 6–8].
In most cases, regressed TGCTs present as metastatic disease, mainly to the retroperitoneum, and the clinical presentation is normally due to extrinsic compression. Gastrointestinal infiltration, as seen in the presented case, is rarely reported [3, 6, 9]. Differential diagnosis can be difficult, as retroperitoneal masses constitute a heterogeneous group of lesions, most of them are malignant tumours. These include rare primary extra-gonadal GCTs, accounting only for 1–2.5% of all GCTs, so a gonadal primary must first be excluded [10]. As the physical exam is often normal, due to the complete regression or small size of reminiscent tumour, ultrasound screening is essential [3, 6].
The diagnosis of testicular tumour regression is histologic, defined by recent WHO criteria, including features within the scar and peripheral area. Pathognomonic signs are thick intratubular calcification in the scar (present in 15% of cases) and germ cell neoplasia in situ (50%) in the periphery [4]. Tumour markers, such as LDH, β-hCG and AFP, are important to the diagnostic approach; however, they are central to staging, treatment and follow-up [1, 3].
The management of burned-out TGCT is similar to non-regressed TGCT, as the regression does not appear to change the prognosis of the clinical stage, and the standard treatment of metastatic disease is surgical resection followed by systemic chemotherapy [1–5]. Orchiectomy is essential to burned-out definition and differential diagnosis with primary extra-gonadal GTC, in addition to be the foundation for proper treatment, because systemic therapy is not completely effective for the testicles due to the haemato-testicular barrier [3, 6, 7].
In conclusion, patients who present with a retroperitoneal mass, diagnosis of metastatic progression of a germ cell neoplasia should be considered, and in male patients, it is mandatory to suspect and rule out a primary testicular tumor.
Conflict of interest statement
None.
References
- ultrasonography
- computed tomography
- chemotherapy regimen
- adolescent
- germ cell tumor
- neoplasm metastasis
- orchiectomy
- retroperitoneal space
- signs and symptoms
- testicular neoplasms
- diagnosis
- duodenum
- neoplasms
- testis
- testicular germ cell neoplasm
- burnout
- young adult
- misdiagnosis
- excision
- testicular examination
- complete remission
- histopathology tests



