-
PDF
- Split View
-
Views
-
Cite
Cite
James Ashcroft, Betania Mahler-Araujo, Richard J Davies, Intersphincteric epidermoid inclusion cyst: report of a rare case, Journal of Surgical Case Reports, Volume 2020, Issue 3, March 2020, rjaa004, https://doi.org/10.1093/jscr/rjaa004
Close - Share Icon Share
Abstract
Epidermoid inclusion cysts of the perineal region are a rare entity, which require appropriate diagnosis and management. Here we describe the unusual case of a large protruding epidermoid inclusion cyst originating from the intersphincteric anal plane, which was mobilized and excised successfully. Essential investigations to ensure accurate diagnosis in addition to surgical technique to reduce recurrence and patient morbidity are described in this case report.
INTRODUCTION
Epidermoid inclusion cysts are uncommon and benign developmental cysts, which progress over time due to incorporation of epidermal tissue into the dermis layer of the skin [1]. They are commonly found in the head and neck region and cause no symptoms at rest; however, these are susceptible to infection and inflammation causing discomfort [1]. In this study, we describe a rare case of an epidermoid inclusion cyst arising between the two anal sphincters and recommend essential investigations and surgical technique to ensure accurate diagnosis and to reduce recurrence and patient morbidity.
CASE REPORT
A 69-year-old male presented to his primary care physician with an 8-year history of a slow-growing large mass protruding from the right anal verge. The patient’s past medical history included a previous basal cell carcinoma, coronary artery disease, atrial fibrillation and diverticular disease. The patient had previously undergone colonoscopic investigation of diverticulosis and underwent polypectomy of the three colonic and one rectal tubular adenoma with low-grade dysplasia a year before. There was no past medical history of trauma to the perineal region or previous perineal procedures. On assessment of the patient at the colorectal unit, the mass originated from the skin of the anal verge and was not involving the anal canal. It was cylindrical in shape, was soft and fluctuant with no irregularities and did not display any overlying cutaneous features. Magnetic resonance imaging (MRI) was undertaken and demonstrated a thin-walled homogenous cystic structure arising in the intersphincteric plane measuring 7 cm × 5 cm × 5 cm (Fig. 1). The cyst was well defined with no invasive features and demonstrated high signal on T2-weighted imaging suggestive of a fluid-filled structure.
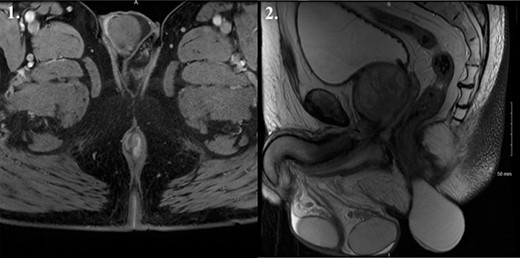
MRI T2 weighted imaging suggestive of a 7 cm × 5 cm × 5 cm fluid-filled structure arising in the intersphincteric plane. 1. Coronal view. 2. Sagittal view.
The cyst was examined under anaesthesia in the lithotomy position and was mobilized into the intersphincteric space and excised preserving the perianal skin (Fig. 2). The cyst was excised entirely and macroscopically appeared to be a thin-walled 8-cm long sac containing a yellow fluid. The resulting skin defect was closed with interrupted 2-0 vicryl dissolvable suture material. Histological analysis of the mass confirmed a large hybrid epidermal inclusion cyst (Fig. 3).

Surgical management of the large intersphincteric epidermoid inclusion cyst. 1. Examination under anaesthesia. 2. Delineation of the origin of the cyst in the intersphincteric plane. 3. Surgical excision of the cyst and haemostasis. 4. Interrupted suture repair of the perineal defect.
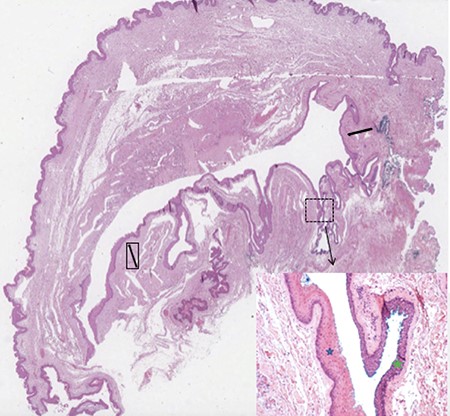
Microscopic overview of the surgical specimen showing a large hybrid epidermal inclusion cyst (black arrows) lined by squamous epithelium (blue star) with areas of transitional epithelium (green star; haematoxylin and eosin stains).
DISCUSSION
Epidermoid inclusion cysts are benign developmental cysts that progress over time due to incorporation of epidermal tissue into the dermis layer of the skin [1]. These epidermal cells form the surrounding walls of the cyst and then secrete the yellow sebum and keratin liquid found in this case [1]. Epidermoid inclusion cysts commonly cause no symptoms at rest; however, these are susceptible to infection and inflammation-causing discomfort [1]. Various factors have been linked to the development of epidermoid cysts including male gender, genetic conditions such as Gardner syndrome (a variant of familial adenomatous polyposis), injury and sun damage to the skin, smoking and the human papillomavirus [1]. The incidence of perineal epidermoid cysts is rare, with the incidence of presacral developmental cysts to be estimated at around 1 in 50 000 [2]. Only one previous case report of an epidermoid inclusion cyst arising between the two anal sphincters in a similar pattern to this case has been described with no clear precipitating factors [3].
It is essential to undertake appropriate investigation such as MRI imaging in cases of suspected epidermoid inclusion cysts. In very rare cases malignant carcinomas may develop from epidermoid cysts as described in five published case reports, necessitating imaging and histopathological analysis [4]. Furthermore, if misdiagnosed and managed as a perianal abscess or fistula-in-ano, there is an estimated post-operative infection rate of ~30% causing significant patient morbidity [1]. Successful epidermoid inclusion cyst removal relies on complete surgical resection and the avoidance of intraoperative surgical spillage due to the potential for recurrence [1]. Care must be taken to avoid anal canal stenosis resulting from excessive excision [1]. The patient in this case had an uneventful post-operative recovery with excellent functional results.
Conflict of interest statement
None.
Funding
None.



