-
PDF
- Split View
-
Views
-
Cite
Cite
Charalambos Menenakos, Hendrik C Albrecht, Stephan Gretschel, Bilateral giant inguinoscrotal hernia. Presentation of a novel combined two-stage repair approach, Journal of Surgical Case Reports, Volume 2020, Issue 3, March 2020, rjaa012, https://doi.org/10.1093/jscr/rjaa012
Close - Share Icon Share
Abstract
Giant inguinoscrotal hernia is typically defined as hernia extending below the midpoint of the inner thigh, in the standing position. These hernias can be a demanding surgical problem as replacing bowel contents into the abdomen that can cause a life-threatening increase in intra-abdominal pressures. Various techniques such as preoperative progressive pneumoperitoneum (PPP), debulking of abdominal contents with visceral resections with or without omentectomy and phrenectomy have been suggested. We report the case of a 65-year-old patient with giant bilateral inguinal hernia. We applied a novel two-stage combined approach consisting of PPP with simultaneous single shot injection of botulinum toxin Type A into the anterior abdominal wall, and a second stage laparotomy with hernia repair (Stoppa technique). This technique makes possible the successful treatment of giant inguinal hernias without the need for visceral resection. To our knowledge, this is the first presented case of this combined treatment modality.
INTRODUCTION
Giant inguinoscrotal hernias are typically defined as those extending below the midpoint of the inner thigh, in the standing position [1, 2].
These types of hernia appear rarely, especially bilaterally, and they are challenging [1].
Several techniques such as visceral debulking, phrenectomy and progressive pneumoperitoneum (PPP) have been described for treatment.
CASE REPORT
A 65-year-old male patient was referred to our hospital with urinary retention. The patient suffered from an intellectual disability and mental retardation.
The CT scan of the abdomen disclosed a complete scrotal shift of both small intestine and sigmoid colon and a bilateral Grade II hydronephrosis (Fig. 1). The patient was then referred to our surgical department for the operative hernia repair.
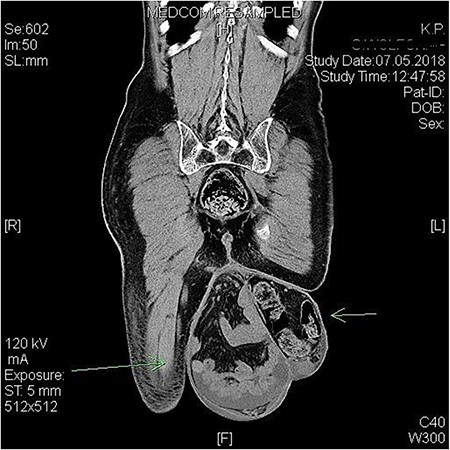
Preoperative CT scan showing the bilateral giant scrotal hernia with massive shift of intestine into scrotum.
Clinically, the hernia reached to a level just above the knees (Akpo Classification 3b) [3] (Fig. 2).

We applied a novel therapeutic concept based on the combination of three separate components, an intra-abdominal catheter [PleurX™ Catheter, Care Fusion, IL, USA] was laparoscopically placed into the abdominal cavity in order to create a PPP. At the same time, an intramuscular injection of 100 IU of botulinum toxin of five doses of 20 IU each was given on each side of the anterolateral abdominal wall. The application was sonographically guided in the space between the abdominal external and internal oblique muscle (Fig. 3).

Intramuscular injection of botulinum toxin under sonographic guidance. The insufflation catheter has been already placed.
Following laparoscopy, a PPP was created with insufflation of room air through the abdominal catheter (1500 ml of room air/day in the first 5 days up to 2000 ml/day for the next 10 days).
We performed a Stoppa procedure as following: median laparotomy with progressive reduction of the viscera without opening the sac. The space behind the rectus muscle, from the internal part of the pubic symphysis and the Cooper ligament to the umbilicus, was prepared. The Retzius space, the iliac vein and artery in the Bogros space, the obturator region and the psoas region were dissected on both sides. One ~20 × 30 cm PVDF Mesh [DynaMesh®-CICAT-Aachen, Germany] was placed into a preperitoneal position according to the standard Stoppa procedure [4]. The scrotum and testicles were intraoperatively examined by our urologists. No orchiectomy was necessary and scrotal skin was left intact (Fig. 4).

Aspect of abdomen and scrotum after completion of surgical repair.
The patient’s postoperative course was uneventful. After a short recovery on the ICU, he was readmitted to the normal surgical ward on the second postoperative day. The patient was released at a stable condition on the 10th postoperative day. Fifteen months after surgery, the patient is doing well.
DISCUSSION
The definition of a giant inguinoscrotal hernia is relatively consistent in the literature. The hernia must extend below the level of the midpoint of the patient’s inner thigh in upright position or should display an anteroposterior diameter of at least 30 cm or a laterolateral diameter of ~50 cm with non-reducibility for >10 years [1].
The prevalence of giant inguinoscrotal hernias in developed countries is very low (2.81–5% of all inguinal hernias). Bilateral giant inguinoscrotal hernias are rarer accounting for only 12.5% of all giant inguinoscrotal hernias [1].
Akpo published the first classification for bilateral giant inguinoscrotal hernias [3]. The condition is rare, more common in men living in rural communities in developing countries, and it has considerable negative impact on the quality of life, but also potentially life-threatening complications.
Akpo studied exactly the sociopsychological factors that push patients to seek medical advice. The main reason why patients presented at the (late) time they presented, was, according to Akpo, purely social, due to coital refusal from the sexual partner or inability to penetrate, which could lead up to a divorce [3].
Surgery is the only treatment. The major challenge surgeon must face is the problem of repositioning herniated viscera to the abdominal cavity. A forced reduction of hernia contents into the contracted peritoneal cavity with prior preparation will mostly cause a fulminant raise of intra-abdominal and intrathoracic pressure, leading to life-threatening complications [4].
Cavalli et al. presented a hug technique for the reduction of displaced viscera. The authors concluded that this technique permits to treat with success giant inguinoscrotal hernia, avoiding the use of further specific procedure [5].
A technique that has been widely used for the remodelling of abdominal cavity prior to hernia repair is the induction of preoperative PPP and it was introduced in 1940 by Goňi Moreno. PPP was first recommended for patients with big incisional hernias and loss of domain, but it has also been used for giant inguinoscrotal hernias with an excessive shift of viscera in scrotum. The technique includes the laparoscopic or percutaneous placement of an intra-abdominal catheter and progressive insufflation of 1–2 L of air for a period of 10–15 days. PPP has a multimodal effect including increase of the capacity of the retracted abdominal cavity; it promotes a pneumatic lysis of intestinal adhesions, allows the reduction of the hernia contents and improves diaphragmatic function. It is contraindicated in patients suffering from cardiac and pulmonary insufficiency and abdominal infections, and it requires a prolonged preoperative hospital stay that ranges from 7 to 18 days.
In our case, we used the PPP along with injection of botulinum toxin in the abdominal wall and a second step with operative repair of the hernia using the Stoppa technique [4]. There are a few studies about use of botulinum toxin for large incisional hernias with loss of domain [6], but no published studies about the application of the toxin for giant scrotal hernias.
To our knowledge, this is the first case of a bilateral giant inguinoscrotal hernia repaired with the combined technique of PPP, injection of botulinum toxin and Stoppa technique. The Stoppa technique uses a giant preperitoneal prosthesis through an infraumbilical midline incision. The Stoppa technique is an established technique for the repair of bilateral inguinal hernias and many studies have shown its clinical efficacy [4]. Our proposed combined two-step technique makes it possible to successfully treat giant inguinal hernias without the need for visceral resection.
CONFLICT OF INTEREST STATEMENT
None declared.



