-
PDF
- Split View
-
Views
-
Cite
Cite
Shota Akabane, Takahisa Oonishi, Tomohiro Takenoue, Tatsunari Kawamoto, Toshiaki Kunimura, A rare trigger for acute appendicitis leading to small bowel obstruction: traditional serrated adenoma of the appendiceal foramen, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz047, https://doi.org/10.1093/jscr/rjz047
Close - Share Icon Share
Abstract
This is the first documented case of traditional serrated adenoma (TSA) of the appendiceal foramen that triggered acute appendicitis resulting in small bowel obstruction (SBO). An 88-year-old Japanese man presented with abdominal pain, distension, and appetite loss. Computed tomography demonstrated distended ileum adherent to cecum with thickened walls. He was diagnosed with SBO, and open ileoceal resection was eventually performed. Pathological examination revealed that a pedunculated polyp had obstructed the appendiceal foramen and triggered acute appendicitis, thus leading to SBO. Histopathological examination of the polyp revealed that the long fronds of the adenoma were lined by dysplastic epithelial cells, which is a characteristic feature of TSA. This case report illustrates that a tiny TSA can trigger the obstruction of the appendiceal foramen and lead to acute appendicitis and SBO. We underline the need for the resection of the polyps in this region regardless of their size.
INTRODUCTION
Appendicitis (inflammation of the vestigial vermiform appendix) is one of the most common causes of acute abdomen and one of the most frequent indications for emergency abdominal surgery worldwide [1]. Appendiceal obstruction is considered the primary cause of appendicitis. Obstruction may be caused by fecalith, calculi, lymphoid hyperplasia, infectious processes, or benign/malignant tumors [2].
Small bowel obstruction (SBO) is also frequently encountered in clinical settings and is caused by various conditions such as postoperative adhesions, mesenteric torsion or inflammatory adhesions [3].
Traditional serrated adenoma (TSA) is a type of serrated polyp that is most commonly found in non-adenomatous polyps. TSAs appear and behave like conventional adenomas, often appear pedunculated, exhibit unequivocal adenomatous dysplasia with branching and budding crypts, and are found more often in the distal colon [4].
In this study, we present a case of acute appendicitis caused by TSA in the appendiceal foramen that results in SBO requiring surgical intervention.
CASE REPORT
An 88-year-old Japanese man presented with abdominal pain, distension, and appetite loss that exacerbated over the last 4–5 days. He also experienced intermittent vomiting prior to hospital admission. His past medical history included myocardial infarction treated with percutaneous catheter intervention, and he was receiving aspirin (100 mg/day) and lansoprazole (15 mg/day). Upon physical examination, the abdomen was diffusely distended and tender; however, there were no signs of peritoneal irritation such as rebound tenderness or muscle guarding. His vital signs were within the normal limits. Laboratory tests revealed slightly elevated inflammatory markers and anemia (white blood cell count: 4400/μL; hemoglobin: 11.4 g/dL; C-reactive protein: 3.189 mg/dL), but tumor marker levels were not elevated (carcinoembryonic antigen: 1.7 ng/mL; carbohydrate antigen 19-9:6.3 U/mL). Computed tomography showed a distended ileum that adhered to the cecum with thickened walls (Fig. 1a and b). There was no evidence of free air, massive ascites, intestinal ischemia or mesenteric torsion. Thus, he was diagnosed with SBO, and a nasogastric tube was inserted to decompress the upper gastrointestinal tract. However, his symptoms continued to persist. We subsequently performed exploratory laparotomy 2 days after admission and detected diffusely dilated intestines and an inflamed cecum that adhered to the ileum. Iliocecal resection including D2 lymph node dissection was accomplished after we took into account the possibility of malignancy. Ileum-ascending colon anastomosis was performed with functional end-to-end anastomosis by using Endo GIATM Reload with Tri-stapleTM Technology (purple 60 mm; Covidien, USA).
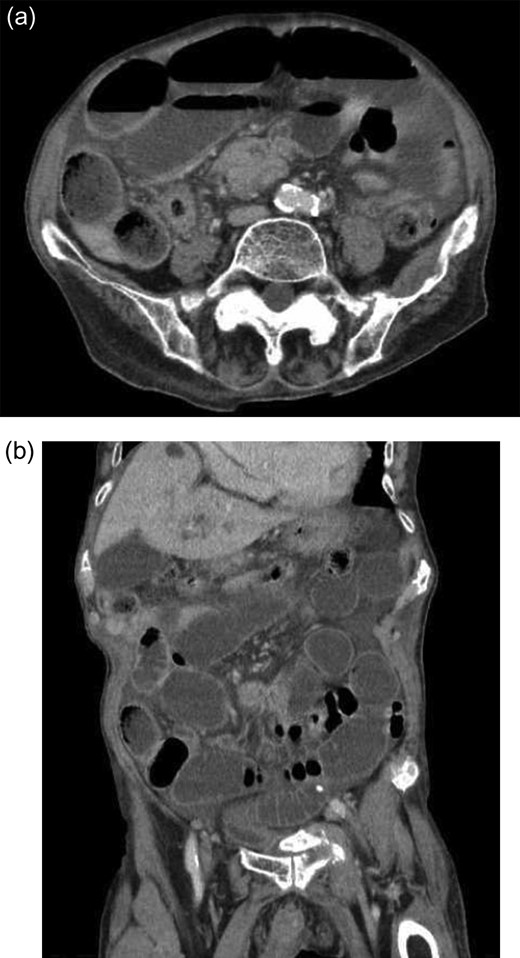
(a and b) Computed tomography showing the distended ileum that adhered to the cecum with thickened walls. There are no signs of free air, massive ascites or intestinal ischemia.
Pathological examination revealed that acute appendicitis and inflammatory adhesions with the ileum led to SBO. There were no other potential triggers of appendiceal foramen obstruction (such as a fecalith) other than a pedunculated polyp, that is ~5 mm in size (Fig. 2a and b). A histopathological examination of the polyp demonstrated that the long fronds of the adenoma were lined by dysplastic epithelial cells characterized by nuclear pleomorphism interspersed with cells containing dystrophic goblet cell vacuoles (Fig. 3a and b); however, there was no evidence of malignancy or invasive growth, in addition to the absence of matured irregular crypts toward normal-appearing nuclei. A pathological examination of the appendix revealed acute inflammation with neutrophil infiltration; the adhesions to the ileum were mainly inflammatory in nature, and no malignancy was observed. On the basis of the clinical course, he was diagnosed with a case of acute appendicitis triggered by the TSA of the appendiceal foramen leading to SBO.
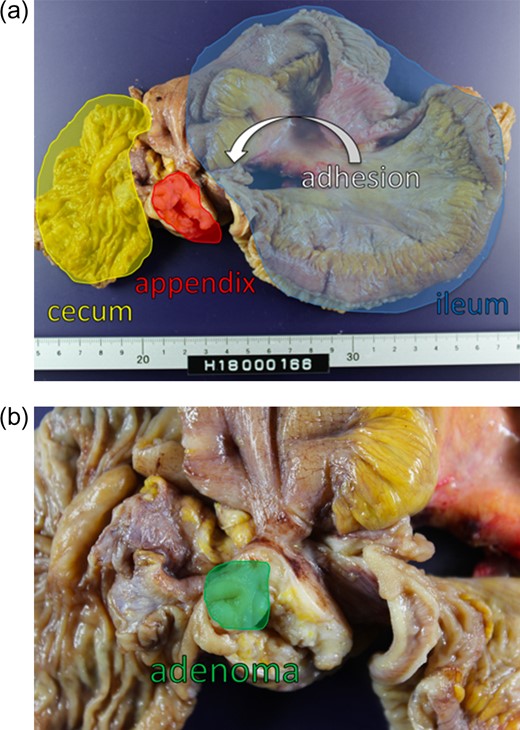
(a and b) Formalin-fixed resected tissue shows no other potential cause of appendiceal foramen obstruction (such as a fecalith) other than a pedunculated polyp that is ~5 mm in size.
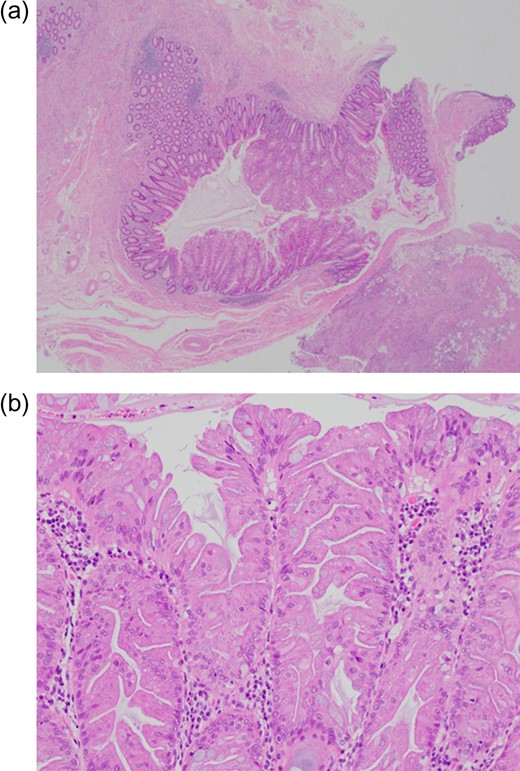
(a and b) Histopathological examination of sections of the polyp showing long fronds of the adenoma lined by dysplastic epithelial cells characterized by nuclear pleomorphism and elongated finger-like villous projections.
The postoperative period was uneventful, and he was discharged 20 days after the operation.
DISCUSSION
There are two distinguishing features of this case. First, the TSA of the appendiceal foramen is a rare entity, and this is the first case report that describes the acute appendicitis caused by the TSA of the appendiceal foramen, which eventually resulted in SBO. Second, this case illustrates that a small polyp can trigger acute appendicitis.
TSA is rarely found near the appendiceal foramen. Serrated polyps are generally the most common non-adenomatous polyps and are classified histologically into three distinct types: hyperplastic polyps (HPs), sessile serrated adenoma/polyps (SSA/Ps) and TSAs. The characteristics of these polyps are described below (Table 1) [5]. Although SSA/Ps have recently been highlighted owing to their particular morphology and distinct oncological behavior, TSAs not only exhibit similar characteristics to those of conventional adenomas but also some interesting behaviors [4]. Nevertheless, TSAs are uncommon and represented <1–2% of all colonic polyps in most studies. In one Japanese study, TSAs accounted for 1.8% of more than 10 000 colonic polyps [6]. These are more common in females and occur much more commonly in the left colon, particularly in the sigmoid colon and rectum [6]. TSAs are characterized by prominent crypt serration with confluent epithelial dysplasia [7]. These polyps are normally pedunculated, may occasionally be large and filiform, and show elongated finger-like villous projections often with inflammation, ulceration, and dilated lymphatic vessels within the lamina propria [7]. Although most pathological characteristics were observed in this case, the TSA of the appendiceal foramen is quite unusual, particularly when it leads to subsequent events. In this respect, there is only one preceding case report that described an SSA/P that led to acute appendicitis and multiple pyogenic liver abscesses [8].
| Features . | Hyperplastic polyp . | Sessile serrated adenoma/polyp . | Traditional serrated adenoma . |
|---|---|---|---|
| Endoscopic appearance | Small, pale | Mucus cap, obscures submucosal vessels | Lobular |
| Most frequent colon site | Distal | Proximal | Distal |
| Shape | Sessile | Sessile | Pedunculated |
| Average size (mm) | <5 | >5 | >5 |
| Irregular crypt bases | − | + | + |
| Gene mutations | |||
| BRAF mutation | +/− | + | +/− |
| K-ras mutation | +/− | − | +/− |
| Malignant potential | − | + (when dysplasia is present) | + |
| Features . | Hyperplastic polyp . | Sessile serrated adenoma/polyp . | Traditional serrated adenoma . |
|---|---|---|---|
| Endoscopic appearance | Small, pale | Mucus cap, obscures submucosal vessels | Lobular |
| Most frequent colon site | Distal | Proximal | Distal |
| Shape | Sessile | Sessile | Pedunculated |
| Average size (mm) | <5 | >5 | >5 |
| Irregular crypt bases | − | + | + |
| Gene mutations | |||
| BRAF mutation | +/− | + | +/− |
| K-ras mutation | +/− | − | +/− |
| Malignant potential | − | + (when dysplasia is present) | + |
| Features . | Hyperplastic polyp . | Sessile serrated adenoma/polyp . | Traditional serrated adenoma . |
|---|---|---|---|
| Endoscopic appearance | Small, pale | Mucus cap, obscures submucosal vessels | Lobular |
| Most frequent colon site | Distal | Proximal | Distal |
| Shape | Sessile | Sessile | Pedunculated |
| Average size (mm) | <5 | >5 | >5 |
| Irregular crypt bases | − | + | + |
| Gene mutations | |||
| BRAF mutation | +/− | + | +/− |
| K-ras mutation | +/− | − | +/− |
| Malignant potential | − | + (when dysplasia is present) | + |
| Features . | Hyperplastic polyp . | Sessile serrated adenoma/polyp . | Traditional serrated adenoma . |
|---|---|---|---|
| Endoscopic appearance | Small, pale | Mucus cap, obscures submucosal vessels | Lobular |
| Most frequent colon site | Distal | Proximal | Distal |
| Shape | Sessile | Sessile | Pedunculated |
| Average size (mm) | <5 | >5 | >5 |
| Irregular crypt bases | − | + | + |
| Gene mutations | |||
| BRAF mutation | +/− | + | +/− |
| K-ras mutation | +/− | − | +/− |
| Malignant potential | − | + (when dysplasia is present) | + |
Acute appendicitis is usually induced by appendiceal obstruction by fecalith, calculi or benign/malignant tumors, including polyps. The efficacy of the endoscopic resection of polyps that are between 5 and 10 mm in size is uncertain regardless of the type of polyp, such as adenoma or hyperplasia [9]. Moreover, it can be risky to resect polyps that are located near the appendiceal foramen because of the thin wall and absence of the muscularis propria [10]. Therefore, the resection criteria tend to vary across facilities. Although appendicitis triggered by a small polyp is uncommon, our experience suggests that it may be worthwhile to consider the resection of incidentally discovered polyps during endoscopy irrespective of the type of the polyp because it is not always easy to endoscopically diagnose polyps that are less than 10 mm in size.
CONFLICT OF INTEREST STATEMENT
None declared.



