-
PDF
- Split View
-
Views
-
Cite
Cite
Jining Dai, Chitrakanti Raja Kapadia, Transverse colon perforation secondary to fish bone ingestion, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjy368, https://doi.org/10.1093/jscr/rjy368
Close - Share Icon Share
Abstract
Accidental ingestion of foreign bodies can be a common occurrence in clinical practice and subsequent perforation is quite rare. The rate of fish bone ingestion is predicted to be higher in some cultures given culinary differences. We report a case of 62-year-old gentleman in rural Australia who had severe left sided abdominal pain and fevers, with a presumptive diagnosis of diverticulitis. Computated tomography revealed intraabdominal abscess. Surgical intervention via laparotomy and right hemicolectomy was performed for an extensive abdominal abscess with a transverse colon perforation and fish bone foreign body in situ (Grunter fish).
INTRODUCTION
Accidental ingestion of fish bones can be common, most of which do no cause complications through the passage of the alimentary canal. The rate of perforation is quite low with reports of <1% of foreign bodies perforating bowel [1, 2]. Due to anatomy of the bowel, the most common site of perforation is at the terminal ileum. Perforation in the large bowel is very uncommon with only a limited number of cases reported. We repot a case with a fish bone related perforated abscess of the transverse colon successfully managed with surgery.
CASE REPORT
A 61-year-old gentleman presented to the emergency department with 4 day history of worsening left sided abdominal pain, localized to the left upper and predominantly left lower quadrant. This was associated with nausea and subjective fevers. He had no changes to his bowel habits and had no vomiting or urinary symptoms. Physical examination revealed a septic picture with a body temperature of 38.4, HR of 110. He was tender in the Left lower quadrant with localized guarding. Laboratory results showed a white cell count of 10.4 × 109 with neutrophils of 7.90 × 109 and a CRP of 127. A CT of the abdomen showed inflammatory changes present involving the transverse colon located left of the midline, this was associated with a low density peripherally enhancing abscess measuring 2.5 × 3 × 2.4 cm (Figs 1 and 2).
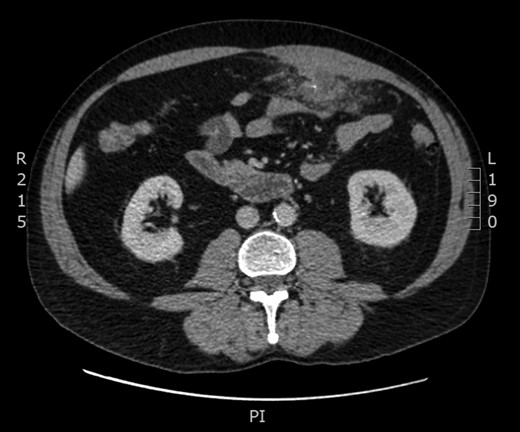
Computated tomography findings with axial image showing inflammatory changes involving the wall of the transverse colon left to the midline with associated abscess. Central opacification consistent with foreign body.
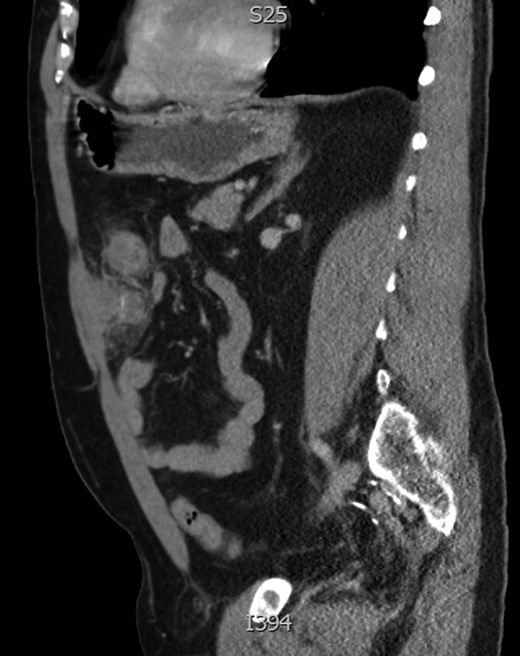
Sagittal image of anterior abdominal collection with central enhancement representing foreign body.
Given these findings, a presumed diagnosis of complicated acute diverticulitis was made and the patient was commenced on antibiotics. Unfortunately, the patients clinical picture failed to improve despite these measures with ongoing fevers and pain. The decision was made for emergency laparotomy. Intraoperatively, a walled off abscess between transverse colon and greater omentum was identified, pulling up towards the abdominal wall. Due to extensive inflammation and location of left part of transverse colon right hemicolectomy was performed with a side to side functional end to end anastomosis created.
Pathology confirmed a subserosal abscess in the greater omentum caused by a fish bone associated with fibrinous peritonitis. The patient’s admission was complicated by post op ileus, atelectasis requiring high flow nasal prongs, thrombocytosis and right upper limb thrombus. He was discharged with follow up after 18 days. On retrospective questioning, the patient had ingested a Grunter fish (Pomadasys argenteus) one week prior to presentation and often without removing bones.
DISCUSSION
Accidental swallowing of foreign bodies can be a common presentation to hospital. Subsequent bowel perforation is rare, and the occurrence of this in large bowel is rarer still [3]. In most cases, ingested fish bones pass through the gastrointestinal tract without causing significant harm or become embedded in the upper digestive tract. 75% of ingested foreign bodies impact at the cricopharyngeal sphincter of the oesophagus and >90% of foreign bodies pass through the intestine if they reach the stomach [4]. With sharp foreign objects, the perforation rate is 15–35% [5].
Of the patients who seek medical attention for ingestion of a foreign body, 80–90% will pass the object without requiring intervention, 10–20% will require endoscopic removal, and <1% will require surgical intervention [6].
Some studies have shown the identification of foreign bodies by plain X-ray can be quite low with sensitivities and specificity of which to be 54.8% and 100%, respectively. In contrast, both sensitivity and specificity of CT scans were 100% [7]. One study showed that the sensitivity of fish bones with plain radiography was as low as 32% [8]. Thus the use of plain radiography to diagnose ingested fish bones may be unreliable and likely dependent on the radiopacity of the ingested item.
Operative management can include a laparoscopic technique [9], however in this case, optical entry may have been problematic due to the presence of anterior adhesions. The approach has been similar in previously documented cases [10].
The diagnosis of foreign body perforation can be difficult and can mimic a wide range of diseases. A systematic approach to patient history and focused examination can help to target diagnostic suspicions and thus arrange the most applicable investigations. The appropriate pre-operative planning can help to decide the most appropriate surgical intervention and thus minimize adverse outcomes for the patient.
Conflict of Interest statement
None declared.



