-
PDF
- Split View
-
Views
-
Cite
Cite
Daichi Nakamura, Yasushi Adachi, Yousuke Kinjo, Shigeki Uchida, Tomohiro Sugiyama, Noriko Sakaida, Michihiko Tsubono, Susumu Ikehara, Extra-gastrointestinal stromal tumor with a large cyst, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjy354, https://doi.org/10.1093/jscr/rjy354
Close - Share Icon Share
Abstract
Gastrointestinal stromal tumors (GISTs) arising at sites other than the alimentary tract are rare, and they are called extra-GISTs (EGISTs). We report a case of a large EGIST forming a cyst, probably arising in the mesentery of the transverse colon. A 64-year-old Japanese man presented to a hospital with an abdominal tumor forming a large cyst. Intraoperatively, the tumor was neither present in nor in contact with the alimentary tract. It was present in the mesentery of the transverse colon and was attached to the greater omentum and peritoneum, immediately anterior to the body of the pancreas. The tumor was resected with the spleen and a part of the pancreas. Histological examination of the tumor revealed that it belonged to the high-risk category of cystic EGISTs.
INTRODUCTION
Although gastrointestinal tumors (GISTs) are rare tumors, the incidence is around 10–20/100 000 population. GISTs are the most common mesenchymal tumors in the alimentary tract [1]. They usually arise in the stomach (60–70%), small intestine (20–30%), and large intestine (10%) [2]. GISTs arising in sites other than the alimentary tract are called extra-gastrointestinal stromal tumors (EGISTs) and are rarer than GISTs; EGISTs arising in the mesentery and omentum account for approximately 2% and 1% of all GISTs, respectively [3, 4].
We report a case of a large cystic EGIST, probably arising in the mesentery of the transverse colon, in an elderly man.
CASE REPORT
A 64-year-old Japanese man consulted our hospital due to an abdominal mass that had persisted for 1 month. He also had a history of appetite and weight loss. He had a past history of a duodenal ulcer and resection of the left adrenal gland due to primary aldosteronism. He had hypertension and paroxysmal atrial fibrillation, as well as rheumatoid arthritis. Computed tomography (CT) revealed a 180-mm tumor in the posterior region of the gastric body (Fig. 1A and B). The tumor consisted of solid and cystic parts. The primary tumor site was unclear on imaging. There was no significant lesion observed in the mucosa of the upper and lower digestive tracts on endoscopic examination.
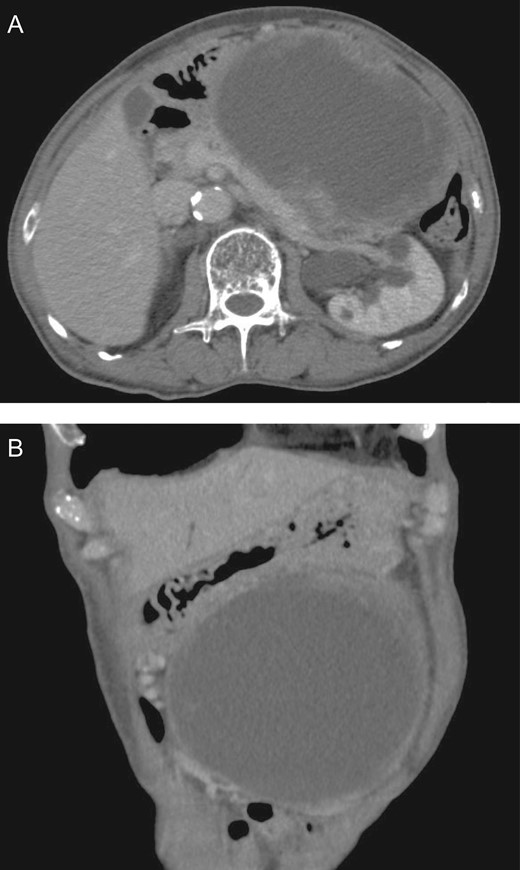
Image of abdominal CT Scan. CT scan revealed a tumor 180 mm in diameter in the region posterior to the gastric body. There was a large cyst in the tumor. Horizontal (A) and coronal (B) sections of the tumor are shown.
Resection of the tumor was carried out. Intraoperatively, the tumor was not in contact with the gastrointestinal tract, but was present in the transverse mesentery immediately anterior to the pancreas, and it seemed to invade the body of the pancreas. The tumor was also in contact with the omentum and peritoneum just anterior to the pancreas. Therefore, the tumor was resected, along with the pancreatic body and tail and the spleen (Fig. 2A and B). The size of the resected tumor was 210 × 200 × 200 mm. There was a large cyst in the tumor (Fig. 2C). The tumor was found to be very close to the pancreas (Fig. 3A). Although the tumor did not invade the pancreas, it was impossible to detach the tumor from the pancreas surgically. Microscopically, the solid component and cyst wall of the tumor showed similar histological features, being mainly composed of mesenchymal spindle cells with plump cigar-shaped nuclei (Fig. 3B and C). Immunohistochemically, the tumor cells were positive for cluster of differentiation (CD)117 (c-Kit) and CD34, and negative for alpha-smooth muscle actin and S100, suggesting that the tumor was an EGIST (Fig. 3D and E). The number of mitotic cells in the tumor was more than 10 cells/50 high-power fields. Based on the size and number of mitotic cells, the EGIST was estimated to be high risk as per the modified Fletcher’s risk classification [5]. Treatment containing oral imatinib for 3 years was planned; however, this treatment unfortunately had to be discontinued after 30 months because of the development of pericarditis. It has been almost 3 years since the surgery, the patient has been well, and no recurrence has occurred.
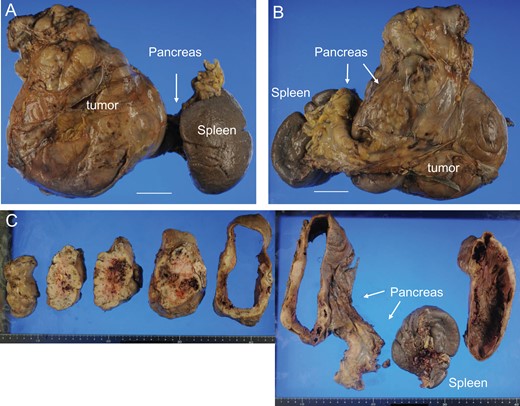
Macroscopic findings of the tumor. Anterior (A) and posterior (B) views of the resected tumor, pancreas, and spleen are shown. Cut sections of the tumor are also shown (C) (Bar = 5 cm). The tumor was resected, along with the pancreas and spleen.
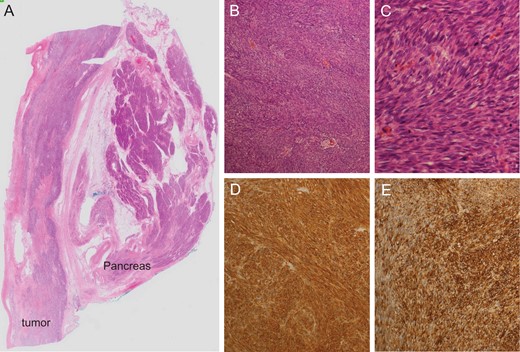
Microscopic findings of the tumor. Loupe image of the tumor and pancreas (A), low-power view (B), high-power view (C) and expression of CD117 (c-kit) (D) and CD34 (E) are shown (B and C, ×10 and ×40 in the objective lens; D and E, ×20 in the objective lens).
DISCUSSION
Most GISTs arise in the alimentary tract, but EGISTs usually arise outside the alimentary tract. It has been reported that EGISTs are histologically similar to GISTs, and they usually express CD117 (c-Kit) similar to GISTs [6]. It is well known that GISTs originate from the interstitial cells of Cajal that express CD117, which originate from the same precursor cells giving rise to smooth muscle cells [7]. Thus, these common precursor cells are most likely the cells of origin in EGISTs [6].
Although GISTs usually appear as a regular solid mass, they rarely present with cyst(s), and large cystic GISTs in particular are extremely rare [1, 2]. The mechanisms of cystic changes in GISTs have been proposed by Bechtold et al. and Zhu et al. and include (i) primary cystic GISTs, (ii) malignant GISTs with cystic degeneration caused by rapid growth of the tumor, (iii) metastatic lesions in the liver or pancreas and (iv) malignant GISTs treated with imatinib [1, 8]. In our case, the EGIST was 210 mm in size on the major axis, and the size (greater than 50 mm) and mitotic cell counts (more than 5 cells/50 high-power fields) were suggestive of EGISTs belonging to the high-risk group. These data suggest that the cyst was formed by degeneration of the tumor, probably owing to insufficient blood supply due to rapid growth. Since the cystic EGIST was close to the stomach and pancreas in our case, it was very difficult to characterize the EGIST before resection. There are several differential diagnoses for cysts in the upper abdominal cavity, such as gastric cystic tumors, pancreatic cystic tumors, omental cysts, mesenteric teratoma, and cystic mesothelioma [2]. Cystic EGISTs should also be considered in the differential diagnoses of cystic lesions in the upper abdominal cavity.
Conflict of Interest statement
None of the authors has any conflicts of interest to declare relevant to this publication.
Funding
No funding was received for this work.



