-
PDF
- Split View
-
Views
-
Cite
Cite
Stacey L Chamberlain, Travis Ackermann, Yuen Chan, Marjan Ghadiri, White mesentery and chylous ascites: an interesting presentation of mesenteric lymphangioma, Journal of Surgical Case Reports, Volume 2019, Issue 12, December 2019, rjz301, https://doi.org/10.1093/jscr/rjz301
Close - Share Icon Share
Abstract
We present an interesting and unusual case of a 57-year-old woman presenting with symptoms concerning for a bowel obstruction, and diagnostic imaging concerning for an internal hernia. The patient underwent an emergency laparotomy and was found to have chylous ascites throughout the abdomen, and the extravasation of chyle into the mesentery giving an appearance of a white mesentery. During this case, we will present all of the findings and discuss the unusual underlying pathology.
INTRODUCTION
Lymphangiomas are rare benign lesions thought to arise from a defect in the lymphatic system with over 60% diagnosed in early childhood [1]. Most commonly, they are found in the neck and axilla, with less than 1% arising from small-bowel mesentery [2].
There are three histologic types of lymphangiomas: simple, cystic and cavernous. Simple or capillary lymphangiomas are usually found in the skin and appear as uniformly small, thin-walled lymphatic spaces on histology. Alternatively, both cystic and cavernous lymphangiomas consist of dilated lymphatic spaces of variable size. The main difference between the cystic and cavernous lymphangiomas is: cystic lesions are associated with collagen and smooth muscle bundles in the stroma, while cavernous lesions tend to be associated with lymphoid stromal tissue [3].
CASE REPORT
A 57-year-old woman presented to our Emergency Department with a short history of abdominal pain, distension and obstipation, associated with nausea.
She denied any previous surgical history and was, otherwise, well with no medical issues. She did not have any systemic symptoms of malignancy and had no known history of liver disease. Of note however, it were similar self-limiting episodes in the past, which had been investigated without any significant findings.
On examination, her vital signs were all within normal limits. Her abdomen was soft and mildly distended, with tenderness notably in the left upper quadrant. Bowel sounds were reduced.
Blood tests revealed a mild leucocytosis of 13.7 × 10^9 g/L (4.0–11.0 × 10^9 g/L) and an elevated lactate of 3.1 mmol/L (0.5–2.0 mmol/L). The remaining laboratory tests were otherwise unremarkable. Her plain abdominal film demonstrated small-bowel dilatation in the upper abdomen, suggestive of a developing bowel obstruction. She proceeded to a computed topography (CT) scan of the abdomen and pelvis that demonstrated a number of findings; these included prominent oedema throughout the small-bowel mesentery associated with enlarged mesenteric lymph nodes, free fluid in the rectovaginal pouch and right iliac fossa, and wall thickening involving most of the jejunum (Fig. 1). The thickened bowel loops and mesenteric oedema were located on the left side of the abdomen, consistent with the patient’s symptoms, and were associated with the impression of a mesenteric swirl, leading to concerns regarding possible internal herniation.

CT demonstrating jejunal wall thickening and mesenteric oedema (arrow).
Therefore, an urgent diagnostic laparoscopy was performed, which required conversion to laparotomy on the discovery of chylous ascites throughout the abdomen without an apparent cause. The proximal 130 cm of jejunal mesentery was found to contain copious extravasated chyle (Fig. 2). The small bowel was viable throughout, with proximal dilatation seen along with a distally collapsed segment without a clear transition point evident. No obvious mass lesions were palpable. An excisional biopsy of a portion of the affected small-bowel mesentery was taken and sent for histopathological analysis. Histology of the small-bowel mesentery showed excessive abnormally dilated thin- and thick-walled lymphatic vessels consistent with a cavernous lymphangioma (Fig. 3).
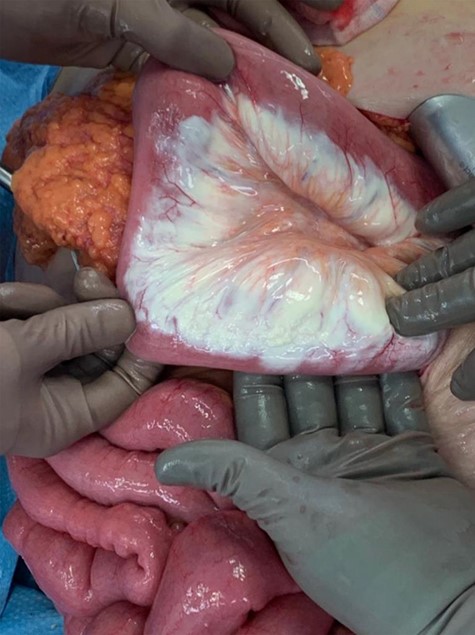
Operative photo demonstrating ‘white mesentery’ (chyle throughout small-bowel mesentery).
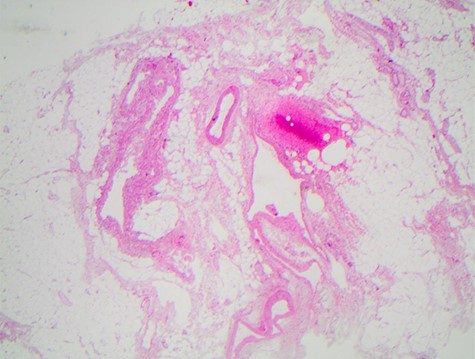
Section of the small-bowel mesentery showing dilated thin- and thick-walled lymphatic vessels, consistent with a cavernous lymphangioma.
Postoperatively, the patient recovered uneventfully and was discharged home on 4 days after surgery. She has remained well on subsequent review up to 3 months later. A panel of tumour markers was sent and revealed an elevated Chromogranin A level of 125 ug/L (27–94 ug/L) at the time of first presentation; however, on subsequent repeat testing 6 weeks later, this had returned to within normal limits (63 ug/L). This transient rise can likely be explained by small-bowel inflammation [4]. To exclude a clinically undetected mass within the root of the mesentery causing lymphatic obstruction, magnetic resonance imaging (MRI) was performed, which showed non-specific small mesenteric lymph nodes and trace free fluid only.
Discussion
There have been multiple case reports of cystic lymphangiomas within the small-bowel mesentery, with a number of presentations ranging from subacute abdominal pain to acute complications, such as intussusception or ischaemia. However, to date, there is only one other report in the literature of a cavernous lymphangioma arising from small-bowel mesentery [5], and to our knowledge, this is the first reported case in which a mesenteric cavernous lymphangioma resulted in chylous ascites and chyle extravasation into the mesentery.
Chylous ascites results from the extravasation of thoracic or intestinal lymph into the abdominal cavity. It is a relatively rare occurrence, with an approximate incidence of 1 per 20 000 admissions [6].
Three potential underlying mechanisms are postulated [7]:
Malignancy causing obstruction of lymph flow and elevated pressure in the intestinal lymph system. This may lead to the damage of the basement membrane, reducing the absorptive ability of the intestinal mucosa and potentially resulting in a protein-losing gastroenteropathy.
Congenital defects (e.g. lymphangiectasia) causing dilated retroperitoneal vessels and fluid extravasation into the peritoneal cavity.
Acquired obstruction due to trauma or iatrogenic injury, resulting in direct leakage of chyle via a lymphoperitoneal fistula.
In a systematic review of 131 studies, atraumatic chylous ascites was most commonly caused by lymphatic abnormalities (32%), malignancy (17%) and cirrhosis (11%). There was also a high prevalence of infective causes such as mycobacterium infection (at 15%), which is indicative of the inclusion of studies from developing countries [8]. Of the cases of chylous ascites due to malignancy, lymphoma is by far the most common cause, accounting for at least one-third to one-half of cases in some reports [6].
We have described an interesting case of a rare pathology presenting in an unusual manner, which is unlike any others in current literature. This case also presented a diagnostic challenge, given the non-specific radiological and surgical findings. It highlights the importance of obtaining biopsies for unexpected and unexplained operative findings.



