-
PDF
- Split View
-
Views
-
Cite
Cite
S Vicente Aguirre, M Mercedes Almagro, Carlos A Romero, Sthefany S Romero, Gabriel A Molina, Ricardo A Buenaño, Giant mesenteric cyst from the small bowel mesentery in a young adult patient, Journal of Surgical Case Reports, Volume 2019, Issue 1, January 2019, rjz002, https://doi.org/10.1093/jscr/rjz002
Close - Share Icon Share
Abstract
Mesenteric cysts are rare tumors, they can emerge from any part of the mesentery of the bowel from the duodenum to the rectum. Their symptomatology can mimic almost any abdominal disease making diagnosis troublesome. In some circumstances, these cysts can grow to considerable sizes making resection almost impossible since its size can compromise different structures. Surgery is the treatment of choice as complete resection is the only curative treatment. We present a case of a female patient, she suffered from recurrent episodes of abdominal pain mistaken as gastritis. After a profound evaluation, a giant mass in her abdomen was identified and successfully treated. Giant primary mesenteric cyst was the final diagnosis.
INTRODUCTION
Mesenteric cysts are rare intra-abdominal tumors [1] that can arise from anywhere in the mesentery from the duodenum to the rectum [2, 3]. Clinical manifestations are extremely varied and non-specific, from asymptomatic patients to severely ill patients with peritonitis, perforation and death [4].
Diagnosis is extremely difficult since its symptomatology can resemble any abdominal disease [1]. Surgery is the treatment of choice, as a complete resection with negative borders is curative and prevents recurrence [4].
We present a case of a 45-year-old patient, a giant cystic mass was identified in her abdomen. After proper evaluation and surgery patient successfully recovered. Giant primary mesenteric cyst was the final diagnosis
CASE REPORT
Patient is a 45-year-old female patient, with past medical history of gastritis. Six months before she sought medical attention, she was complaining of mild upper abdominal pain, however, due to her previous condition she was medicated with proton pump inhibitors assuming that the pain was due to her gastritis. In the last 3 months, she noticed a mass in her upper abdomen and the pain became more severe and started to affect her daily activities, thus she presented to a routine physical exam. No weight loss or other constitutional symptoms were noticed. Also no history of malignancy in her family was mentioned. On clinical examination, a 12 × 15 cm2 mass was discovered on her upper abdomen, mild pain was found on palpation but no tenderness was present. An abdominal ultrasonography revealed a 15 × 15 cm2 septate thin-walled giant cystic mass, it was anechoic and had a volume of ~735 ml. The cyst occupied most of the hepatorenal space and it was in intimate contact with the liver, right kidney and pancreas (Fig. 1A). Due to the size of the mass, CT was requested, it revealed well-defined 19.7 × 15 × 10 cm3 giant cyst, the cyst was located within the small bowel mesentery and it was in intimate contact with the liver, gallbladder, pancreas and right kidney (Fig. 2A). Nevertheless, the tomography could not rule out that the mass had some sort of communication with the bile duct or the pancreas. This is why a magnetic resonance cholangiopancreatography found that the cyst was attached but had no communication with the bile duct or the pancreas (Fig. 3A). CBC and blood work was normal.
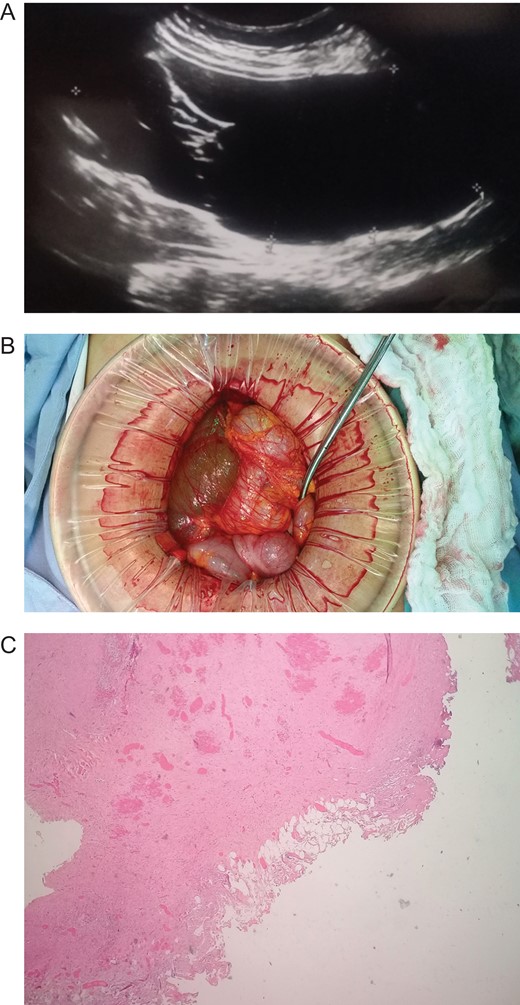
(A) Echography revealing a 15 × 15 cm2 septate thin-walled giant cystic mass. (B) Giant cyst was near the root of the small bowel mesentery. (C) Pathology, cyst wall, without areas of malignancy. (Hematoxylin and eosin staining 10×).

(A) CT revealing a well-defined 19.7 × 15 × 10 cm3 giant cyst. (B) Giant cyst surrounded by the bowel. (C) Pathology, cyst wall covered by adipose tissue. (Hematoxylin and eosin staining 40×.)
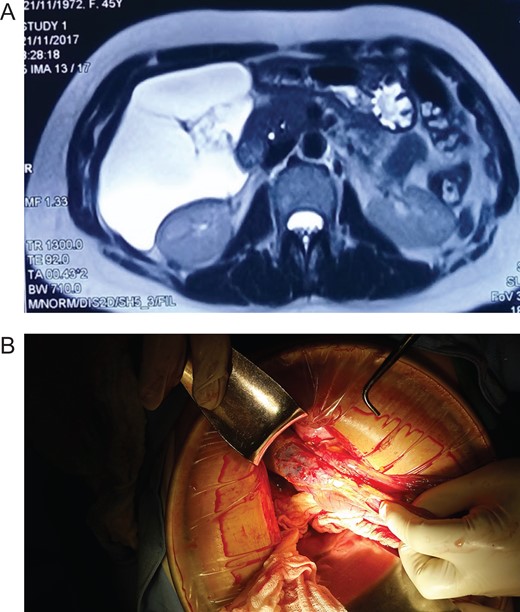
(A) MRI, showing a giant cyst without communication with the bile duct or pancreas. (B) Mesenteric cyst adhesions to the gallbladder and liver.
Due to the size of the cyst and clinical condition surgery was planned. At laparotomy, a 19 × 15 × 10 cm3 mesenteric cyst was discovered (Fig. 1B), the cyst was near the root of the small bowel mesentery but did not compromise its main vessels, it had a yellowish appearance (Fig. 2B), and clear fluid was found within the cyst. Multiple adhesion were identified between the cyst wall and the transverse colon, liver, third portion of the duodenum and gallbladder. With these findings surgery was straightforward, complete resection of the cystic mass was performed, however, the cyst wall was completely attached to the body of the gallbladder and could not be resected without compromising it (Fig. 3B), so a cholecystectomy was performed as well. After this, the remainder of the procedure continued without any complication.
Pathology reported a giant primary mesenteric cyst, it was lined with a single layer of cuboidal epithelial cells and partially covered by adipose tissue and prominent vasculature, it had a yellowish wall and its thickness varied between 0.1 and 0.3 cm (Fig. 1C). Its interior had a white trabecular internal surface with brown patches it did not have any communication with other organs, and no areas of malignancy were found (Fig. 2C).
In the early postoperative period, a tachycardic patient with severe abdominal pain and tenderness was encountered, she became hypotensive an oliguric, thus an emergency re-laparotomy was performed. The 1000 ml of hemoperitoneum was encountered and after extensive washing of the abdominal cavity, an arterial vessel from the resected gallbladder was discovered and successfully managed. After this surgery patient fully recovered. Sips of liquids were initiated on the third postoperative day, and full diet was initiated a day after. She was discharged without any complications and, on follow up controls patient is doing well.
DISCUSSION
Mesenteric cysts are rare intra-abdominal tumors, since the first case was reported in 1507 by Benevieni, <1000 cases have been reported. They appear in 1 in 27 000 to 1 in 250 000 patients [1, 4].
Mesenteric cysts more commonly appear in Caucasians, around the fourth decade with a slightly female preponderance [4]. The origin of the cyst is unknown, while there are many theories including; a continual growth of congenitally malformed or malpositioned lymphatic tissue, secondary to trauma, degenerating lymph nodes or a failure of the leaves of the mesentery to fuse properly. These diversities of theories suggests more than one etiological mechanism may be involved in the development of mesenteric cysts [1, 2, 4].
More than half 60% of the mesenteric cysts arise from the small bowel mesentery, but they had been located anywhere in the mesentery from the duodenum to the rectum [3]. Most cysts are single but can be uni or multilocular. They vary in size and shape from a few centimeters to a size that can occupy most of the peritoneal cavity [1, 4]. Mesenteric cysts are classified on their etiology and pathological features in six groups: cysts of lymphatic origin [3], as we discovered in our case, mesothelial origin, enteric origin, urogenital origin and pseudocysts [2]. Malignancy can appear in any cyst and is reported to be ~3%, however, when there are solid components in the cyst, malignancy rates may be higher [1]. Clinical manifestation are extremely varied and non-specific, from asymptomatic patients to severely ill patients with indistinguishable symptoms of an acute abdomen [3]. This will depend on the characteristics of the cyst, size, location and complications. These complications are fortunately rare but may include intestinal obstruction, volvulus, peritonitis, shock, hemorrhage and death [1, 5]. In our patient, abdominal pain and a mass were discovered that lead to the diagnosis of a giant mesenteric cyst. Chylous cysts are usually associated with the small bowel mesentery, serous cysts usually appear in the mesocolon, and hemorrhagic cysts are caused by trauma and can appear anywhere in the bowel [1]. Preoperative diagnosis is almost impossible based on clinical grounds, as there are no pathognomonic signs or symptoms for mesenteric cysts [6]. Ultrasound and CT can detect the location and size of the lesion, septation, debris, fluid levels and the thickness of the wall. Magnetic resonance imaging (MRI) has been found to be more precise in the evaluation of cyst [6]. In our patient, MRI helped us in preoperative planning of the cyst [5, 7]. The treatment of choice for Mesenteric cysts is surgery. Aspiration and marsupialization are not recommended because they are associated with high recurrence and infection rate [7]. Localized resection of the intestine or surrounding structures may be required to excise the cyst en bloc [4]. As it happened in our case. Laparoscopy may be feasible for cyst removal, and result in less postoperative pain, a shorter hospital stay, and earlier return to normal activity and work [3, 8]. The prognosis for mesenteric cysts is generally good because most are benign and the recurrence rate is low with complete excision [9]. Although mesenteric cysts are rare abdominal tumors, they must always be considered in the differential diagnosis of a patient with abdominal manifestations by all surgeons. Mesenteric cysts should always be assessed with a complete medical history, a thorough clinical examination and accurate complementary exams including blood and radiological investigations. Complete surgical excision of the cyst is the treatment of choice, this avoids recurrence and possible malignant transformation. Laparoscopic surgery in recent years has proven to be an effective alternative technique against these lesions. Also in a unique way, this case proved us, that these tumors can grow to giant sizes making treatment more difficult and that close postoperative follow up is crucial as prompt interventions could reduce morbidity and mortality.
Conflict of Interest statement
None declared.
Funding
The authors received no specific funding for this work.



