-
PDF
- Split View
-
Views
-
Cite
Cite
Rita Dorantes-Heredia, Daniel Motola-Kuba, Carlos Murphy-Sanchez, Carlos D Izquierdo-Tolosa, Jose M Ruiz-Morales, Spontaneous regression as a ‘burned-out’ non-seminomatous testicular germ cell tumor: a case report and literature review, Journal of Surgical Case Reports, Volume 2019, Issue 1, January 2019, rjy358, https://doi.org/10.1093/jscr/rjy358
Close - Share Icon Share
Abstract
Testicular germ cell tumors (TGCTs) are the most frequent type of cancer in young adults. An exceptional event is the spontaneous regression (SR) of the primary tumor. Herein, we describe a burned-out non-seminomatous TGCT case and relevant literature review. A 34-year-old male presenting with low back pain was found to have a retroperitoneal mass upon urotomography. During workup, a heterogeneous testicular mass was evident, and its biopsy showed findings that support the diagnosis of spontaneous tumoral regression. The patient underwent unilateral orchiectomy and a chemotherapy protocol was later initiated, with 85% regression of the retroperitoneal metastatic mass. No progression of the primary tumor has been found. The etiology of SR across different cancer types appears to be associated with the host’s immune response and an angiogenic disturbance of the tumor microenvironment. The burned-out phenomenon is a rare event that needs further research into its molecular sequencing.
INTRODUCTION
Testicular germ cell tumors (TGCTs) are the most frequent type of cancer in young men. They occur particularly in young adults and teenagers aged between 15 and 35 years. Among the histological patterns of the disease, the non-seminomatous TGCT (NS-TGCT) is the most frequent type, having a peak incidence at 25 years [1].
The burned-out testicular tumor represents a germ cell testicular tumor that has spontaneously regressed and commonly manifests as metastasis to the retroperitoneal region [2]. Even though TGCTs possess a considerable histological heterogeneity, tumor regression of the testis is rare [3]. In a recent retrospective study of consecutive patients who had been diagnosed with an NSGCT, the incidence of burned-out tumors was 1% (4 of 621 patients), all of whom were cured [4]. We present one of these rare cases of a testicular burned-out tumor with retroperitoneal masses and no palpable lesion on testicular examination.
CASE PRESENTATION
A 34-year-old male came to the emergency room presenting with moderate to severe low back pain that limited ambulation and was partially controlled with the administration of non-steroidal anti-inflammatory drugs. He had a previous chemonucleolysis of L5–S1 due to a discopathy, and radicular compression of the nerve and left renal enlargement, all found on magnetic resonance imaging (MRI). Otherwise, his clinical history was unremarkable. Abdominal examination did not reveal any discomfort or palpable mass. Lumbar movements and palpation only reproduced the same discomfort, which was also evident upon asking the patient to perform Valsalva’s maneuvers. Both testicles were found normal upon inspection and palpation. The rest of the physical examination was unremarkable.
The lumbar spine MRI obtained previous to the chemonucleolysis reported a discopathy and lymph node enlargement in the retroperitoneal area. Although the discopathy was resolved, the persistence of lumbar pain called for a different approach. During the workup, an urotomography scan was performed, which confirmed multiple retroperitoneal masses in the left paraaortic region measuring 10 × 8 × 6 cm3. There were satellite lymph nodes around the retroperitoneal mass and the left psoas causing lateral displacement of the left kidney, compressing the pyelocaliceal system conditioning hydronephrosis (Fig. 1). Next, a testicular sonogram showed the left testicular heterogeneous parenchyma, with high vascularity and irregular borders, with a size of 28 × 23 × 14 mm3 and a volume of 4.9 cm3. Evaluation of the right testicle was unremarkable. These findings were suggestive of a primary TGCT. Laboratory studies revealed a serum alpha fetoprotein of 15 115 ng/dL (normal value <20 ng/dL), β-human chorionic gonadotropin (β-HCG) of 11 IU/L (normal <0.5 IU/L) and lactate dehydrogenase of 394 U/L (normal value <250 U/L). As part of treatment, the patient underwent left radical orchiectomy without any complication and the specimen was sent for histological analysis. Pathology results showed subtotal atrophy of the testis with extensive fibrosis, multifocal calcifications, focal hemorrhage and Leydig’s cell hyperplasia. Extensive recent hemorrhage in the spermatic cord and epididymis was evident, without pathological alterations. There was no evidence of germ cell tumor, confirming spontaneous tumor regression (Fig. 2). After reassessment, a cystourethroscopy with placement of a double J catheter was performed to resolve the secondary hydronephrosis due to obstructive uropathy. Subsequently, the patient began first-line chemotherapy with four cycles of bleomycin, etoposide and cisplatin (BEP) protocol. Hiccups, nausea, constipation and alopecia presented as adverse events that were managed with symptomatic medications. By the time of the submission of this case report, the patient had concluded his fourth BEP administration.

Urotomography scan with evidence of a retroperitoneal mass that displaces the left kidney with hydronephrosis. The calculated volume was 10 × 8 × 6 cm3.
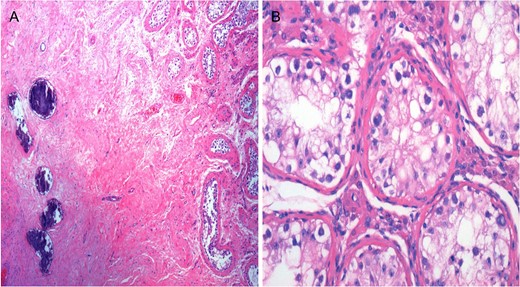
Spontaneous tumor regression in testis. Hematoxylin and eosin (H&E) stain. (A) Pathology results showed subtotal atrophy of the testis with extensive fibrosis, multifocal calcifications, focal hemorrhage and Leydig’s cell hyperplasia. (B) Absent spermatogenesis in seminiferous tubules. Intratubular germ cells with clear cytoplasm.
DISCUSSION
Spontaneous regression (SR) is defined as the partial or complete disappearance of a tumor without any treatment, which is generally perceived as irrelevant to the progression of cancer. This does not account for the tumor’s cure or disappearance [5, 6].
Four SR subtypes are currently reported [5]: (i) regression of primary tumor, which is associated with hemorrhagic tumor or emboli of the renal vein showing fibrosis, hyalinization, calcification or ossification; expressed antigens are keratins, epithelial mucin antibody, carcinoembryonic antigen and vimentin; (ii) regression of metastases; (iii) prolonged remission; and (iv) delayed metastases.
Burned-out TGCT clinical presentation varies according to metastatic deposits, and includes abdominal palpable mass (47%), loin pain (35%) and transient testicular pain (29%) as the most common symptoms; the regressed testicular lesion is not appreciable on physical exam [3]. These signs and symptoms are principally due to extrinsic pressure of the retroperitoneum and explain why stage III TGCTs may be identified at a late disease onset [7]. Differential diagnosis of burned-out TGCT includes extra gonadal germ cell tumors, which are rare, with a frequency of 5–10% of all TGCTs, with the retroperitoneal region being the most frequent site [8].
However, if scarring is seen in the testis, the possibility of germ cell tumor regression must be considered [9]. This incident is histologically defined by scar formation, intratubular calcifications, lymphoplasmacytic infiltrates, macrophages rich in hemosiderin and testicular atrophy [7]. These patients may also present with reduced spermatogenesis and microlithiasis [10]. Part of the diagnostic challenge is defining whether the studied neoplasm is of primary or secondary origin. This raises the importance of testicular assessment when a retroperitoneal mass is discovered. Metastatic findings secondary to the burned-out tissue have similar prognosis as a primary TGCT [7].
Aside from TGCT, renal cell carcinoma and melanoma are frequently described with SR. Based on the behavior and response to treatment of these two neoplasms, we can assume that factors associated with SR are related to the immune response to the tumor’s microenvironment and deprivation of the tumor’s blood supply. Being activated immune retaliation presumably the most important trigger [5, 6].
CONCLUSIONS
A ‘burned-out’ TGCT is an exceptional finding but in the presence of a retroperitoneal mass, testicular assessment should be considered. It is important to notice that SR of the tumor does not appear to change the prognosis of the clinical stage.
Our current understanding of SR is derived from other neoplasms that exhibit a similar behavior. Furthermore, many ‘burned-out’ TGCT cases lack molecular sequencing. This fact can hinder our knowledge of this phenomenon; thus, further research is needed.
CONFLICT OF INTERESTS
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
FUNDING
The author(s) received no financial support for the research, authorship and/or publication of this article.
ETHICAL APPROVAL
Our institution does not require ethical approval for reporting individual cases or case series.
INFORMED CONSENT
Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.



