-
PDF
- Split View
-
Views
-
Cite
Cite
Motomu Suito, Takeshi Kitazawa, Ikkei Takashimizu, Tsuneko Ikeda, Madelung’s disease: long-term follow-up, Journal of Surgical Case Reports, Volume 2019, Issue 1, January 2019, rjy356, https://doi.org/10.1093/jscr/rjy356
Close - Share Icon Share
Abstract
Madelung’s disease (MD) is a rare lipid metabolic disorder of adipose tissue overgrowth, which has been reported to be related to alcohol abuse. Although it does not affect survival itself, alcoholism and metabolic disorders associated with MD can be life-threatening. Although surgical procedures and classifications have been reported, long-term follow-up has rarely been reported. Here, we report a 61-year-old Japanese man with MD who has been followed-up for 12 years. Lipectomy was performed three times over the first 3 years and a total of 4 kg of adipose tissue was excised. Relapse has not been observed. He was diagnosed with multiple hepatocellular carcinomas (MHC) and placed on dialysis due to hepatorenal syndrome caused by alcoholism. Moreover, one of the MHC ruptured resulting in hemorrhagic shock. The cause of death in MD is not fat proliferation but comorbidities. Long-term observation and multidisciplinary systemic management are necessary for MD patients.
INTRODUCTION
Madelung’s disease (MD), also known as multiple symmetric lipomatosis, Launois-Bensaude syndrome and benign symmetric lipomatosis, is a rare disorder of adipose metabolism [1]. MD lesions do not affect survival, but comorbidities can be life-threatening [2]. There have been few reports of long-term follow-up in MD. Here, we report a case of MD with 12-year follow-up since initial surgery.
CASE PRESENTATION
A 61-year-old Japanese man presented to our hospital with growing subcutaneous tumors on his shoulders, upper arms, chest and back. He had first noticed the lesions on his shoulders 5 years previously, and they appeared gradually on his upper arms, chest and back (Fig. 1).

Preoperative physical examination (61 years old: body weight 63 kg). Symmetrical, painless, bulging soft masses were seen on the posterior neck, shoulders, upper arms, chest and back.
He had alcoholic cirrhosis, hypertension, hyperlipidemia and hyperuricemia, and was a smoker (30 cigarettes/day×41 years). He did not have diabetes mellitus, neuropathy, or viral hepatitis and his family history was negative.
Physical examination revealed symmetrical, painless, bulging soft masses on the posterior neck, shoulders, upper arms, chest and back. Computed tomography (CT) showed that the lesions were due to fat accumulation and alcoholic cirrhosis was revealed.
Biopsy was performed and histopathological examination showed adipose tissue without malignancy. With a clinical diagnosis of MD, the patient was scheduled for surgical treatment.
The fatty masses on the shoulders, upper arms and back were excised on the deep fascia including redundant loose skin (excision weight: 1315 g). The adipose tissue was white, slightly large, uniform in size, brittle and non-encapsulated (Fig. 2a). Histopathological examination showed relatively small adipose cells without malignancy (Fig. 2b).
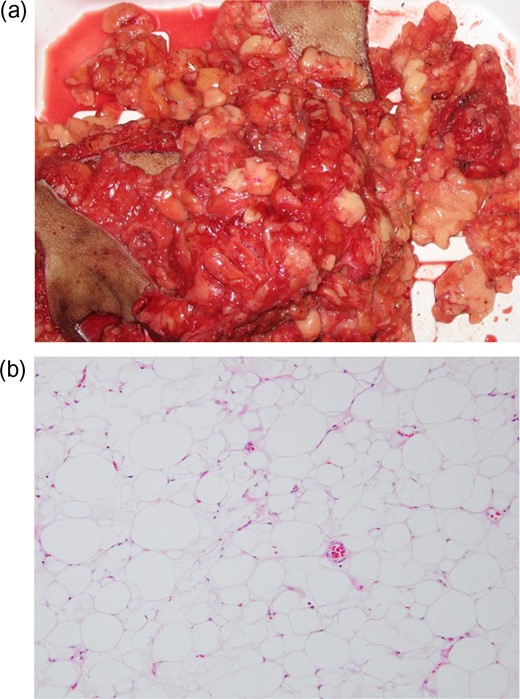
(a) Resected fatty masses. The adipose tissue was white, slightly large, uniform in size and brittle. (b) Histopathological findings (hematoxylin and eosin staining, original magnification ×100). Histopathological examination showed relatively small adipose cells with a slight increase in vascular elements without malignancy.
We performed further lipectomy in the same areas at 62 and 63 years old (excision weights: 1755 and 970 g, respectively). He has been followed-up by observation because he refused additional surgery. Although alcoholism did not improve, no obvious relapse has occurred postoperatively (Fig. 3).

Postoperative physical examination (63 years old, 3 months after third lipectomy: body weight 70 kg). The lesions on both shoulders, upper arms and back were reduced. Postoperative wounds were less remarkable.
At 69 years old, hepatorenal syndrome due to end-stage cirrhosis gradually worsened. At 73 years old, he began to receive artificial dialysis and was diagnosed with multiple hepatocellular carcinomas (MHC) due to alcoholic liver cirrhosis. In the same year, one of the MHC lesions ruptured and he developed hemorrhagic shock. Hepatic arterial chemotherapy was performed. Cure of MHC is impossible and treatment plan is discussed. The lesions themselves have not changed in size, but skin relaxation was remarkable (Fig. 4).

Postoperative physical examination (73 years old, 12 years after initial surgery: body weight 55 kg) There were no changes in size of the lesions themselves, but skin relaxation was remarkable.
DISCUSSION
MD is a rare disorder of adipose metabolism, presenting with multiple, symmetrical, non-encapsulated fatty masses in the maxillofacial region, neck, shoulder, trunk, limbs and other areas [1]. MD occurs frequently in middle-aged men with the highest rate in Mediterranean countries and a low rate in Asia [3]. Most cases are sporadic, and risk factors and pathophysiology remain unknown [4]. However, alcoholism is considered to contribute to MD development [2, 4].
Schiltz et al. [5] divided MD into five phenotypes (Fig. 5), and our case was classified as type Ic. They hypothesized that fat proliferation starts in the neck and spreads toward the lower body. In our case, the lesions were first noticed on both shoulders and spread toward the upper arms and back. However, it was possible that fat proliferation had occurred in his neck prior to his becoming aware of it. Moreover, as the lesions did not spread to the lower body since visiting our hospital 5 years after onset, he was classified as type Ic. Ramos et al. [6] reported that prior to a period of stabilization or quiescence of the lesion, there is a period of rapid growth. Further investigation of the maturation time of these lesions is necessary as this will be important for anticipating the clinical course and determining treatment.
![The different phenotypes and subtypes of the classification (from reference [5] and partially modified) Phenotype I (subtypes: a, b, c), Phenotype II, Phenotype III.](https://oupdevcdn.silverchair-staging.com/oup/backfile/Content_public/Journal/jscr/2019/1/10.1093_jscr_rjy356/2/m_rjy356f05.jpeg?Expires=1772331588&Signature=K8HIbYBod7ANbePwCFRbC3~87mrNNJpkrpEuWt~G5CuT2jgzSv9QQ-s6Qo9kBjKNC2DNF~z7ChkDqzV5CIMnIutevMxePbgV650VYjMU~qTDwiLRZiKLmxzU00-Oc2K2NCPdmqZSEt7hTPoW~qzTnV39fKp9IyudpapvX2z2dEjeRzLuqlyhtJDIYqNPiZBmU72n8bqMy5cGTkr1LCSYv7RsVXF~SPhbJy64yRFvFhbYnjjBfUhroePKU16eGLwc6~XkvcA1GG5qn5gO~Nxf~cnKvbR~hVNFZepKFoBoyk-mDXY2Y3fLbwGsF8ZfscL~a~6uojWHC1lCRN~JRiV0ig__&Key-Pair-Id=APKAIYYTVHKX7JZB5EAA)
The different phenotypes and subtypes of the classification (from reference [5] and partially modified) Phenotype I (subtypes: a, b, c), Phenotype II, Phenotype III.
Cosmetic deformity, mobility complaints, and compression symptoms, such as dyspnea and dysphagia, are indications for treatment [1], and surgical resection is the only effective therapeutic option [1]. Lipectomy and liposuction have been reported as surgical methods [1]. The former has been performed more widely than the latter due to its direct visualization, extensive debulking [7], and lack of special equipment requirements. We performed the former and excised the lesions including redundant loose skin. During surgery, it was difficult to determine the boundary between the lesion and normal fat because there was no capsule. We distinguished the lesions based on the following characteristics: white, slightly large, uniform in size and brittle. Postoperative cosmetic outcome was acceptable, and obvious relapse has not been observed 12 years postoperatively.
Relapse in the same or different location was reported as a frequent event [8], and average time until relapse was 3.8 years [9]. Even with alcohol withdrawal and weight reduction, it is impossible to reverse or stop the progression of adipose tissue overgrowth [1, 7, 8]. Therefore, long-term observation is needed and re-operation is considered if the lesions relapse. In photographs 12 years after initial surgery, the lesions appear to have remained unchanged in size, but the normal fat and muscles were atrophic (Fig. 4). There may be relationship between stabilization of the lesion in size and continuation of drinking alcohol. In addition, to the best of our knowledge, although there have been many studies on MD patients [1, 6], the relationship between patient's age and the rate of postoperative adipose tissue overgrowth remains unknown. Because many of these studies had a short follow-up period, they did not report whether relapse occurred or not.
Comorbidities, such as metabolic disorders, dyslipidemia, hypertension, chronic obstructive pulmonary disease, hypothyroidism and diabetes mellitus have been reported [8]. As MD is more common in patients with alcohol dependence, MD patients frequently have hepatic disease [8]. Lüscher et al. [2] reported that the cause of death in MD patients was not fat deposition but comorbidities. In our case, alcoholism did not improve and one of the MHC lesions that occurred due to alcoholic cirrhosis ruptured.
The most common treatment approach for alcoholism is initial intensive inpatient or outpatient care based on 12-step principles, followed by continuing care involving self-help groups, 12-step group counseling, or individual therapy [10]. Telephone-based counseling and brief counseling are effective as forms of step-down continuing care after an initial stabilization treatment [11]. In our case, although it was proposed to treat the patient’s alcoholism, it has been left up to the patient and his family since his visitation. Alcohol consumption sharply decreased with the deterioration of physical condition.
Once a diagnosis of MD has been made, multidisciplinary systemic management with other departments is important along with surgical treatment.
CONCLUSION
Death in MD patients is not due to fat proliferation but to comorbidities. Long-term observation and multidisciplinary systemic management are necessary for MD patients.
CONFLICT OF INTEREST STATEMENT
No potential COI to disclose.



