-
PDF
- Split View
-
Views
-
Cite
Cite
M Tarazi, F T Tomalieh, A Sweeney, D Sumner, Y Abdulaal, Literature review and case series of haemorrhagic cholecystitis, Journal of Surgical Case Reports, Volume 2019, Issue 1, January 2019, rjy360, https://doi.org/10.1093/jscr/rjy360
Close - Share Icon Share
Abstract
A diagnosis of haemorrhagic cholecystitis is difficult to make as it is rare and mimics other common disorders. We present three patients who presented with haemorrhagic cholecystitis, two of whom were on anti-coagulation at presentation. All 3 patients were treated conservatively, 2 with percutaneous cholecystostomy drainage and 1 patient with intravenous antibiotics. There are few guidelines on the management of such a condition.
INTRODUCTION
A diagnosis of haemorrhagic cholecystitis is difficult to make as it is rare and the presentation mimics other more common disorders—typically acute cholecystitis. We report three non-consecutive, single-centre cases of haemorrhagic cholecystitis and a review of the literature. Causes of haemorrhagic cholecystitis are rare especially if there is no known underlying pathology.
CASE 1
An 87-year-old gentleman presented to Accident and Emergency Department (A&E) with a 5-day history of sharp right iliac fossa pain aggravated by movement and a productive cough. There was no associated vomiting, bowels were normal but he had a reduced appetite for the last week.
The patient had a complex past medical history, with asymptomatic IgG kappa myeloma, chronic obstructive pulmonary disease, ischaemic heart disease and previous pulmonary emboli. He was on Warfarin with target INR of 3–4. His surgical history was a previous appendicectomy. Prior to admission he was under investigation for a gastrointestinal stromal tumour.
On examination there was a small palpable mass and tenderness in the right iliac fossa, PR examination was unremarkable. Observations were stable and he was apyrexial.
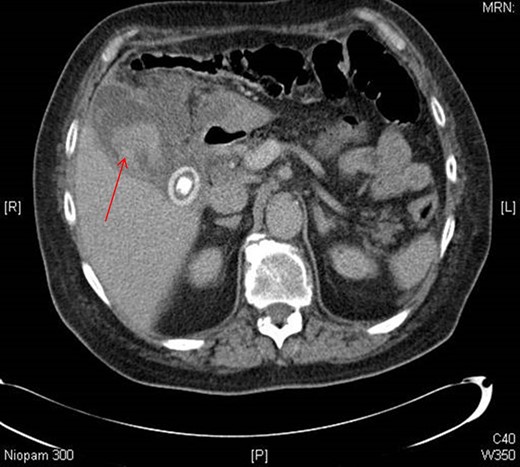
Initially on admission he was managed as an infective exacerbation of COPD. Blood tests revealed a macrocytic anaemia (Hb 108 g/L), neutrophilia (8.8 g/L) with a WCC of 11.1 × 109 L, slightly deranged liver function (bilirubin 21 μM, AST was 50 iU/L) and CRP of 236 mg/L. At the time of presentation INR was 7.8. CT abdomen/pelvis showed pericholecystic inflammatory change, in keeping with cholecystitis, with hyper-attenuation in the gallbladder, suggestive of haemorrhage (Fig. 1).
Following this he underwent percutaneous cholecystostomy and 300 ml of blood was drained. He was treated with IV antibiotics. The patient was discharged and was well on follow up.
CASE 2
A 65-year-old lady presented to A&E with a 2-day history of nausea and generalized upper abdominal pain. She denied any fevers, vomiting or urinary symptoms but had not opened her bowels for 2 days. She had a past medical history of hypothyroidism, atrial fibrillation, polycystic kidney disease and a previous ovarian cystectomy. She was on warfarin with a target INR of 2–3.
On examination she had a soft, moderately distended abdomen with tenderness in the right lumbar region. Bloods revealed a WCC of 10.5 × 109 L, deranged liver function tests (Bilirubin 21 μM, AST 114 iU/L and an ALP of 156 iU/L) and INR 2.8.
She was treated initially for an acute appendicitis, and a CT abdomen/pelvis revealed a distended gallbladder containing an acute haemorrhage, which was further characterized with an abdominal ultrasound. The decision was taken to treat conservatively with antibiotics. She was discharged 5 days later and underwent elective cholecystectomy.
CASE 3
A 92-year-old lady presented to A&E with a 1-day history of severe intermittent sharp right upper quadrant and epigastric pain with a single episode of bilious vomiting. She had also noticed a tender abdominal mass in the right upper quadrant.
She had a past medical history of renal transitional cell carcinoma, diverticular disease, anaemia, glaucoma, hiatus hernia and had previously undergone a hysterectomy. She was not on any anti-coagulation.
On examination she was tender in the right upper quadrant. Bloods showed raised inflammatory markers (WCC 26 × 109 L, Neutrophils 24 g/L and CRP 192 mg/L) and ALP (186 iU/L) with an INR of 1.1.
She was initially treated with IV antibiotics for biliary sepsis and underwent an ultrasound scan which showed possible acute cholecystitis, with an oedematous thick-walled gallbladder but no gallstones visualized.
CT abdomen/pelvis showed gross distention of the gallbladder with an oedematous wall measuring up to 4 mm in thickness. There was a suspected defect noted in the posteroinferior gallbladder wall suspicious for perforation and an ill-defined hyperdensity within the gallbladder lumen with no gallstones identified. There was a moderate volume of free fluid in the pelvis.
She had a percutaneous cholecystostomy inserted, where heavily bloodstained bile was drained initially and then haemoserous fluid, she was discharged home on oral antibiotics with the drain in-situ. On review in clinic 4 weeks post discharge she was clinically well with no ongoing pain and the drain was removed.
DISCUSSION
Whilst acute cholecystitis is a common presentation, haemorrhagic cholecystitis is a rare complication which presents with symptoms of right upper quadrant pain and positive Murphy’s sign [1]. The pathogenesis is not fully understood, but it is theorized that transmural inflammation leads to ischaemia and erosion of the gallbladder mucosa, which can lead to haemobilia [2–4].
The aetiology is not fully understood, however there are some causes reported in the literature, such as chronic renal failure, gallbladder neoplasm, haemophilia and vasculidities [5, 6]. Patients with haemorrhagic cholecystitis commonly have other medical co-morbidities with many either taking anticoagulants or steroids, which increases the likelihood of haemorrhage into the gallbladder [7, 8].
Diagnosis of haemorrhagic cholecystitis is challenging as haemorrhage in the gallbladder is often difficult to image using conventional methods [9]. CT shows wall thickening of the distended gallbladder and heterogenous materials inside the gallbladder, whilst ultrasound can also be used to visualize hyperechoic contents in the gallbladder [3].
Cholecystectomy on actively infected or inflamed gallbladders may increase risk of complications [10], therefore in many cases a percutaneous cholecystotomy can be performed. Previous literature suggests that the use of cholecystostomy can be less successful than cholecystectomy with repeat CT showing hyperdense contents in the gallbladder [3]. Another potential option is to treat conservatively with antibiotics and withholding anti-coagulant therapy.
Reviewing the literature, 30 case reports of 31 patients were identified presenting with haemorrhagic cholecystitis between 1985 and 2018. In total, 45% were found to be on anti-coagulation vs. 45% not on any anti-coagulation (10% were not reported). Most patients (22, 71%) were treated with a cholecystectomy compared to three patients (10%) were treated with a percutaneous cholecystostomy drainage, five patients (16%) were treated conservatively with intravenous antibiotics, and one patient (3%) was treated with endoscopic nasobiliary drainage. All published papers in the literature are summarized in Table 1.
| Author . | Year of publication . | Journal . | Patient age/gender . | Anti-coagulation . | Treatment choice . |
|---|---|---|---|---|---|
| Liefman et al. | 2018 | International Annals of Medicine | 73 F | Y—Rivaroxaban | Conservative with IV antibiotics, elective lap chole |
| Lopez et al. | 2018 | Radiology | 84 M | Not mentioned | Laparoscopic Cholecystectomy |
| Berndtson et al. | 2017 | Surgical Infections Case Reports | 75 F | N | Open Cholecystectomy |
| Choi et al. | 2017 | Trauma Image & Procedure | 65 M | N | Laparotomy + Open Cholecystectomy |
| Kinnear et al. | 2017 | BMJ Case Reports | 74 M | Y—Apixaban | Laparotomy + Open Cholecystectomy |
| Shishida et al. | 2017 | Case Reports in Gastroenterology | 79 M | Y—Heparin for dialysis | ERCP and ENBD |
| Oshiro et al. | 2017 | International Surgery | 61 F | Y—Warfarin | Conservative with IV antibiotics, elective lap chole |
| Yoshida et al. | 2017 | J-Stage | 73 M | Y | Laparoscopic Cholecystectomy |
| Espino et al. | 2016 | Cirugía Española | 59 M | N | Laparotomy + Open Cholecystectomy |
| Cho et al. | 2015 | Korean Journal of Thoracic and Cardiovascular Surgery | 61 M | Y—Warfarin | Cholecystostomy drainage |
| Aljiffry et al. | 2014 | Journal of Surgical Case Reports | 57 M | N | Cystic artery embolization + Open Cholecystectomy |
| Matsukiyo et al. | 2014 | J-Stage | 68 F | Y—thrombolysis | Laparotomy + Open Cholecystectomy |
| Seok et al. | 2013 | Korean Journal of Internal Medicine | 84 M | N | Laparoscopic Cholecystectomy |
| Taniguchi et al. | 2013 | J-Stage | 48 M | Y—Heparin for dialysis | Laparotomy + Open Cholecystectomy |
| Kwon et al. | 2012 | Korean Journal of Hepatobiliary Pancreatic Surgery | 75 M | Y—Warfarin | Laparoscopic Cholecystectomy |
| García-Pérez et al. | 2011 | Revista Española De Enfermedades digestivas | 24 F | N | Lap to Open Cholecystectomy + intra-opertaive cholangiography |
| Jung et al. | 2011 | Journal of the Korean Surgical Society | 55 M | N | Laparoscopic Cholecystectomy |
| Parekh et al. | 2010 | JAMA Surgery |
|
|
|
| Lin et al. | 2010 | Journal of Internal Medicine of Taiwan | 80 M | Y—Warfarin | Laparoscopic Cholecystectomy |
| Chen et al. | 2010 | The American Journal of the Medical Sciences | Elderly M | Y—Heparin | Laparoscopic Cholecystectomy |
| Miyamoto et al. | 2009 | J-Stage | 42 F | N | Conservative with IV antibiotics, elective lap chole |
| Oh et al. | 2009 | Journal of the Korean Society of Magnetic Resonance in Medicine | 40 M | Not mentioned | Laparoscopic Cholecystectomy |
| Lai et al. | 2009 | Journal of Chinese Medical Association | 81 M | Y—Heparin for dialysis | Conservative with IV antibiotics, elective lap chole |
| Morris et al. | 2008 | Case Reports in Gastroenterology | 91 F | N | Open Cholecystectomy |
| Pandya et al. | 2008 | Abdominal Imaging | 85 F | Y—Warfarin | Conservative with IV antibiotics |
| Kim et al. | 2007 | World Journal of Gastroenterology | 55 M | N | Cholecystostomy drainage |
| Gremmels et al. | 2004 | Journal of Ultrasound in Medicine | 66 M | N | Laparotomy + Open Cholecystectomy |
| Hanaki et al. | 2000 | J-Stage | 66 M | Not mentioned | Laparotomy + Open Cholecystectomy |
| Stempel et al. | 1993 | Journal of Vascular and Interventional Radiology | 78 M | Y—Heparin during AAA repair | Cholecystostomy drainage |
| Brady et al. | 1985 | Disease of the Colon & Rectum | 79 M | N | Open Cholecystectomy |
| Author . | Year of publication . | Journal . | Patient age/gender . | Anti-coagulation . | Treatment choice . |
|---|---|---|---|---|---|
| Liefman et al. | 2018 | International Annals of Medicine | 73 F | Y—Rivaroxaban | Conservative with IV antibiotics, elective lap chole |
| Lopez et al. | 2018 | Radiology | 84 M | Not mentioned | Laparoscopic Cholecystectomy |
| Berndtson et al. | 2017 | Surgical Infections Case Reports | 75 F | N | Open Cholecystectomy |
| Choi et al. | 2017 | Trauma Image & Procedure | 65 M | N | Laparotomy + Open Cholecystectomy |
| Kinnear et al. | 2017 | BMJ Case Reports | 74 M | Y—Apixaban | Laparotomy + Open Cholecystectomy |
| Shishida et al. | 2017 | Case Reports in Gastroenterology | 79 M | Y—Heparin for dialysis | ERCP and ENBD |
| Oshiro et al. | 2017 | International Surgery | 61 F | Y—Warfarin | Conservative with IV antibiotics, elective lap chole |
| Yoshida et al. | 2017 | J-Stage | 73 M | Y | Laparoscopic Cholecystectomy |
| Espino et al. | 2016 | Cirugía Española | 59 M | N | Laparotomy + Open Cholecystectomy |
| Cho et al. | 2015 | Korean Journal of Thoracic and Cardiovascular Surgery | 61 M | Y—Warfarin | Cholecystostomy drainage |
| Aljiffry et al. | 2014 | Journal of Surgical Case Reports | 57 M | N | Cystic artery embolization + Open Cholecystectomy |
| Matsukiyo et al. | 2014 | J-Stage | 68 F | Y—thrombolysis | Laparotomy + Open Cholecystectomy |
| Seok et al. | 2013 | Korean Journal of Internal Medicine | 84 M | N | Laparoscopic Cholecystectomy |
| Taniguchi et al. | 2013 | J-Stage | 48 M | Y—Heparin for dialysis | Laparotomy + Open Cholecystectomy |
| Kwon et al. | 2012 | Korean Journal of Hepatobiliary Pancreatic Surgery | 75 M | Y—Warfarin | Laparoscopic Cholecystectomy |
| García-Pérez et al. | 2011 | Revista Española De Enfermedades digestivas | 24 F | N | Lap to Open Cholecystectomy + intra-opertaive cholangiography |
| Jung et al. | 2011 | Journal of the Korean Surgical Society | 55 M | N | Laparoscopic Cholecystectomy |
| Parekh et al. | 2010 | JAMA Surgery |
|
|
|
| Lin et al. | 2010 | Journal of Internal Medicine of Taiwan | 80 M | Y—Warfarin | Laparoscopic Cholecystectomy |
| Chen et al. | 2010 | The American Journal of the Medical Sciences | Elderly M | Y—Heparin | Laparoscopic Cholecystectomy |
| Miyamoto et al. | 2009 | J-Stage | 42 F | N | Conservative with IV antibiotics, elective lap chole |
| Oh et al. | 2009 | Journal of the Korean Society of Magnetic Resonance in Medicine | 40 M | Not mentioned | Laparoscopic Cholecystectomy |
| Lai et al. | 2009 | Journal of Chinese Medical Association | 81 M | Y—Heparin for dialysis | Conservative with IV antibiotics, elective lap chole |
| Morris et al. | 2008 | Case Reports in Gastroenterology | 91 F | N | Open Cholecystectomy |
| Pandya et al. | 2008 | Abdominal Imaging | 85 F | Y—Warfarin | Conservative with IV antibiotics |
| Kim et al. | 2007 | World Journal of Gastroenterology | 55 M | N | Cholecystostomy drainage |
| Gremmels et al. | 2004 | Journal of Ultrasound in Medicine | 66 M | N | Laparotomy + Open Cholecystectomy |
| Hanaki et al. | 2000 | J-Stage | 66 M | Not mentioned | Laparotomy + Open Cholecystectomy |
| Stempel et al. | 1993 | Journal of Vascular and Interventional Radiology | 78 M | Y—Heparin during AAA repair | Cholecystostomy drainage |
| Brady et al. | 1985 | Disease of the Colon & Rectum | 79 M | N | Open Cholecystectomy |
| Author . | Year of publication . | Journal . | Patient age/gender . | Anti-coagulation . | Treatment choice . |
|---|---|---|---|---|---|
| Liefman et al. | 2018 | International Annals of Medicine | 73 F | Y—Rivaroxaban | Conservative with IV antibiotics, elective lap chole |
| Lopez et al. | 2018 | Radiology | 84 M | Not mentioned | Laparoscopic Cholecystectomy |
| Berndtson et al. | 2017 | Surgical Infections Case Reports | 75 F | N | Open Cholecystectomy |
| Choi et al. | 2017 | Trauma Image & Procedure | 65 M | N | Laparotomy + Open Cholecystectomy |
| Kinnear et al. | 2017 | BMJ Case Reports | 74 M | Y—Apixaban | Laparotomy + Open Cholecystectomy |
| Shishida et al. | 2017 | Case Reports in Gastroenterology | 79 M | Y—Heparin for dialysis | ERCP and ENBD |
| Oshiro et al. | 2017 | International Surgery | 61 F | Y—Warfarin | Conservative with IV antibiotics, elective lap chole |
| Yoshida et al. | 2017 | J-Stage | 73 M | Y | Laparoscopic Cholecystectomy |
| Espino et al. | 2016 | Cirugía Española | 59 M | N | Laparotomy + Open Cholecystectomy |
| Cho et al. | 2015 | Korean Journal of Thoracic and Cardiovascular Surgery | 61 M | Y—Warfarin | Cholecystostomy drainage |
| Aljiffry et al. | 2014 | Journal of Surgical Case Reports | 57 M | N | Cystic artery embolization + Open Cholecystectomy |
| Matsukiyo et al. | 2014 | J-Stage | 68 F | Y—thrombolysis | Laparotomy + Open Cholecystectomy |
| Seok et al. | 2013 | Korean Journal of Internal Medicine | 84 M | N | Laparoscopic Cholecystectomy |
| Taniguchi et al. | 2013 | J-Stage | 48 M | Y—Heparin for dialysis | Laparotomy + Open Cholecystectomy |
| Kwon et al. | 2012 | Korean Journal of Hepatobiliary Pancreatic Surgery | 75 M | Y—Warfarin | Laparoscopic Cholecystectomy |
| García-Pérez et al. | 2011 | Revista Española De Enfermedades digestivas | 24 F | N | Lap to Open Cholecystectomy + intra-opertaive cholangiography |
| Jung et al. | 2011 | Journal of the Korean Surgical Society | 55 M | N | Laparoscopic Cholecystectomy |
| Parekh et al. | 2010 | JAMA Surgery |
|
|
|
| Lin et al. | 2010 | Journal of Internal Medicine of Taiwan | 80 M | Y—Warfarin | Laparoscopic Cholecystectomy |
| Chen et al. | 2010 | The American Journal of the Medical Sciences | Elderly M | Y—Heparin | Laparoscopic Cholecystectomy |
| Miyamoto et al. | 2009 | J-Stage | 42 F | N | Conservative with IV antibiotics, elective lap chole |
| Oh et al. | 2009 | Journal of the Korean Society of Magnetic Resonance in Medicine | 40 M | Not mentioned | Laparoscopic Cholecystectomy |
| Lai et al. | 2009 | Journal of Chinese Medical Association | 81 M | Y—Heparin for dialysis | Conservative with IV antibiotics, elective lap chole |
| Morris et al. | 2008 | Case Reports in Gastroenterology | 91 F | N | Open Cholecystectomy |
| Pandya et al. | 2008 | Abdominal Imaging | 85 F | Y—Warfarin | Conservative with IV antibiotics |
| Kim et al. | 2007 | World Journal of Gastroenterology | 55 M | N | Cholecystostomy drainage |
| Gremmels et al. | 2004 | Journal of Ultrasound in Medicine | 66 M | N | Laparotomy + Open Cholecystectomy |
| Hanaki et al. | 2000 | J-Stage | 66 M | Not mentioned | Laparotomy + Open Cholecystectomy |
| Stempel et al. | 1993 | Journal of Vascular and Interventional Radiology | 78 M | Y—Heparin during AAA repair | Cholecystostomy drainage |
| Brady et al. | 1985 | Disease of the Colon & Rectum | 79 M | N | Open Cholecystectomy |
| Author . | Year of publication . | Journal . | Patient age/gender . | Anti-coagulation . | Treatment choice . |
|---|---|---|---|---|---|
| Liefman et al. | 2018 | International Annals of Medicine | 73 F | Y—Rivaroxaban | Conservative with IV antibiotics, elective lap chole |
| Lopez et al. | 2018 | Radiology | 84 M | Not mentioned | Laparoscopic Cholecystectomy |
| Berndtson et al. | 2017 | Surgical Infections Case Reports | 75 F | N | Open Cholecystectomy |
| Choi et al. | 2017 | Trauma Image & Procedure | 65 M | N | Laparotomy + Open Cholecystectomy |
| Kinnear et al. | 2017 | BMJ Case Reports | 74 M | Y—Apixaban | Laparotomy + Open Cholecystectomy |
| Shishida et al. | 2017 | Case Reports in Gastroenterology | 79 M | Y—Heparin for dialysis | ERCP and ENBD |
| Oshiro et al. | 2017 | International Surgery | 61 F | Y—Warfarin | Conservative with IV antibiotics, elective lap chole |
| Yoshida et al. | 2017 | J-Stage | 73 M | Y | Laparoscopic Cholecystectomy |
| Espino et al. | 2016 | Cirugía Española | 59 M | N | Laparotomy + Open Cholecystectomy |
| Cho et al. | 2015 | Korean Journal of Thoracic and Cardiovascular Surgery | 61 M | Y—Warfarin | Cholecystostomy drainage |
| Aljiffry et al. | 2014 | Journal of Surgical Case Reports | 57 M | N | Cystic artery embolization + Open Cholecystectomy |
| Matsukiyo et al. | 2014 | J-Stage | 68 F | Y—thrombolysis | Laparotomy + Open Cholecystectomy |
| Seok et al. | 2013 | Korean Journal of Internal Medicine | 84 M | N | Laparoscopic Cholecystectomy |
| Taniguchi et al. | 2013 | J-Stage | 48 M | Y—Heparin for dialysis | Laparotomy + Open Cholecystectomy |
| Kwon et al. | 2012 | Korean Journal of Hepatobiliary Pancreatic Surgery | 75 M | Y—Warfarin | Laparoscopic Cholecystectomy |
| García-Pérez et al. | 2011 | Revista Española De Enfermedades digestivas | 24 F | N | Lap to Open Cholecystectomy + intra-opertaive cholangiography |
| Jung et al. | 2011 | Journal of the Korean Surgical Society | 55 M | N | Laparoscopic Cholecystectomy |
| Parekh et al. | 2010 | JAMA Surgery |
|
|
|
| Lin et al. | 2010 | Journal of Internal Medicine of Taiwan | 80 M | Y—Warfarin | Laparoscopic Cholecystectomy |
| Chen et al. | 2010 | The American Journal of the Medical Sciences | Elderly M | Y—Heparin | Laparoscopic Cholecystectomy |
| Miyamoto et al. | 2009 | J-Stage | 42 F | N | Conservative with IV antibiotics, elective lap chole |
| Oh et al. | 2009 | Journal of the Korean Society of Magnetic Resonance in Medicine | 40 M | Not mentioned | Laparoscopic Cholecystectomy |
| Lai et al. | 2009 | Journal of Chinese Medical Association | 81 M | Y—Heparin for dialysis | Conservative with IV antibiotics, elective lap chole |
| Morris et al. | 2008 | Case Reports in Gastroenterology | 91 F | N | Open Cholecystectomy |
| Pandya et al. | 2008 | Abdominal Imaging | 85 F | Y—Warfarin | Conservative with IV antibiotics |
| Kim et al. | 2007 | World Journal of Gastroenterology | 55 M | N | Cholecystostomy drainage |
| Gremmels et al. | 2004 | Journal of Ultrasound in Medicine | 66 M | N | Laparotomy + Open Cholecystectomy |
| Hanaki et al. | 2000 | J-Stage | 66 M | Not mentioned | Laparotomy + Open Cholecystectomy |
| Stempel et al. | 1993 | Journal of Vascular and Interventional Radiology | 78 M | Y—Heparin during AAA repair | Cholecystostomy drainage |
| Brady et al. | 1985 | Disease of the Colon & Rectum | 79 M | N | Open Cholecystectomy |
CONCLUSION
Haemorrhagic cholecystitis is a rare diagnosis following a common presentation of symptoms and there are few guidelines on the management of such a condition. In cases such as these the patient’s condition and co-morbidities must be taken into account when deciding on management options.
CONSENT
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests and no sources of funding.



