-
PDF
- Split View
-
Views
-
Cite
Cite
Paul R Burchard, Alan A Thomay, Appendiceal intussusception in the setting of ulcerative colitis, Journal of Surgical Case Reports, Volume 2018, Issue 4, April 2018, rjy044, https://doi.org/10.1093/jscr/rjy044
Close - Share Icon Share
Abstract
Appendiceal intussusception is a very rare condition with an estimated incidence of 0.01%. Most cases present in adults with chronic waxing and waning of symptoms over a period of weeks to months. We report a case of a 39-year-old Caucasian female with a 5-week history of worsening right-sided abdominal pain. Computed tomography revealed cecal thickening without visualization of the appendix. A colonoscopy revealed mild diffuse erythema and edema in the ascending colon as well as a mass within the lumen of the cecum. Biopsies of the colon were suggestive of mild ulcerative colitis (UC). The patient’s symptoms continued and laparoscopic assisted ileocecectomy was performed revealing an inverted appendix protruding into the cecal lumen. The patient was discharged without any complications and began mesalamine therapy for her UC.
INTRODUCTION
Appendiceal intussusception is a very rare condition that affects all ages, with most reported cases in adults (76%) [1]. Clinical presentation varies, with some reports mimicking acute appendicitis and others with chronic abdominal pain. When identified in adults, care must be taken to rule out neoplasia and avoid improper removal. We report a case of appendiceal intussusception in the setting of ulcerative colitis (UC) and discuss the clinical features, diagnostic workup and operative management of this condition together with a review of the literature.
CASE REPORT
A 39-year-old Caucasian female presented with a 5-week history of worsening right-sided abdominal pain, which she described as sharp and burning, without radiation. There were no associated fevers, chills, nausea, vomiting, diarrhea or hematochezia. She initially attributed her symptoms to starting a new diet while vacationing in Italy, however, her symptoms had persisted since returning to the USA. On presentation to an outside facility, it was thought her symptoms were a result of stool retention. Laxatives and regular bowel movements provided no relief. Past medical history was notable for chronic abdominal pain and a previous colonoscopy performed 6 years ago for complaints of painless hematochezia was without masses, polyps or inflammation. Family history included colon cancer in her maternal grandfather. On physical examination, her temperature was 36.3°C and other vital signs were normal. Her abdomen had normal bowel sounds in all four quadrants with mild tenderness to palpation in the right upper and right lower quadrants without guarding or rigidity. No lymphadenopathy was noted. Laboratory values were notable for a white blood cell count of 4.3.
CT with oral and IV contrast demonstrated cecal thickening without visualization of the appendix (Fig. 1). A colonoscopy was performed, which showed mild diffuse erythema and edema in the last 40 cm of the ascending colon as well as a mass within the lumen of the cecum (Fig. 2). Biopsies of the colon demonstrated chronic active colitis and ulceration of the cecal mass, suggestive of mild UC (Fig. 3, bottom right and left). No granulomata were present, and there was no evidence of dysplasia. The decision was made for operative management due to continuation of her symptoms and need for definitive diagnosis.

CT with oral and IV contrast of the abdomen and pelvis in axial (A), coronal (B) and sagittal (C) views.
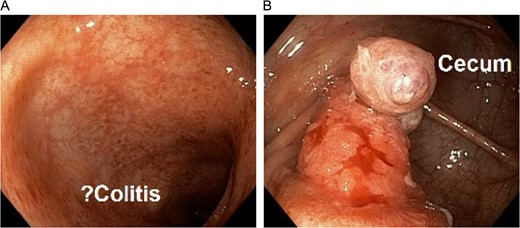
Colonoscopy demonstrating questionable active colitis in the ascending colon (left) and a mass in the cecum (right).
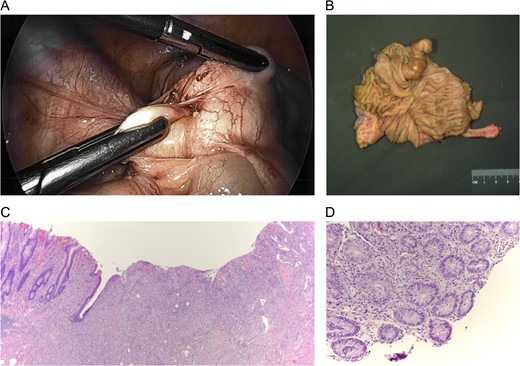
(Top left) Laparoscopic identification of the cecum with invagination of the appendix. (Top right) Ileocecectomy gross specimen with intussuscepted appendix within the cecum. (Bottom left) Microscopic section of the appendix with ulceration of the mucosa. (Bottom right) Biopsy of left colon demonstrating cryptitis and crypt abscesses.
Laparoscopic assisted ileocecectomy was performed revealing an inverted appendix protruding into the cecal lumen (Fig. 3, top Left and right). The patient recovered quickly and without complications and is currently taking mesalamine for her UC.
DISCUSSION
This patient presented with appendicitis due to appendiceal intussusception in the setting of UC. In her case, the appendix had completely invaginated into the cecum. The association of appendiceal intussusception with UC has not been described in previous literature. We hypothesize that her recent flare of UC resulted in inflammatory changes of the appendix and peri-appendiceal lymph nodes that provided a lead point for intussusception.
Intussusception results from invagination of bowel into the lumen of an adjacent segment of bowel. This is often due to lesions within the bowel lumen acting as ‘lead points’ during normal peristalsis [2]. In adults, these lead points are pathologic in 90% of cases with malignancies accounting for approximately 65% [3]. The mesenteric vascular supply of the intussuscepted segment can become compromised, resulting in ischemia of the bowel wall and symptoms of colicky pain.
Appendiceal intussusception has an estimated incidence of 0.01%, with most adult cases resulting from endometriosis (33%), inflammation (19%), mucoceles (19%), adenomas (11%), carcinoids (7%) or adenocarcinomas (6%) [1, 4, 5]. Most patients present with chronic waxing and waning of symptoms over a period of weeks to months. The most common symptoms are abdominal pain (78%), vomiting (26%), blood per rectum (23%), and diarrhea (13%) or constipation (10%) [1]. The diagnosis can be made using double-contrast barium enema, ultrasound, CT scan or endoscopy. In this case, CT scan showed a target sign, which is classic for intussusception. In addition, endoscopy suggests intussuscepted appendix and biopsies demonstrated nearby UC.
Recent literature recommends appendectomy with resection of the cecal cuff [1]. This provides a margin for resection of the appendix and reduces the risk of recurrences. Some case studies have reported colonoscopic appendectomy using endoloop ligation [6, 7], while others have reported resolution of symptoms using a barium enema [8, 9].
In this case, concern for possible neoplasm and inability to reduce the appendiceal intussusception, rather than ulcerative colitis, led to a larger resection.
CONFLICT OF INTEREST STATEMENT
None declared.



