-
PDF
- Split View
-
Views
-
Cite
Cite
Tracy R Geoffrion, Linde DeKeyzer, Gopi Shah, Suja J Nair, Timothy J Pirolli, Kemp Kernstine, Pulmonary paraganglioma in a 10-year-old: a case report and review of the literature, Journal of Surgical Case Reports, Volume 2018, Issue 4, April 2018, rjy047, https://doi.org/10.1093/jscr/rjy047
Close - Share Icon Share
Abstract
Paraganglioma is a rare extra-adrenal tumor of the paraganglia often found in association with sympathetic and parasympathetic nerves. The case presented is of a 10-year-old boy with hemoptysis who was found to have an obstructive bronchial mass. He underwent surgical resection and biopsy confirmed primary pulmonary paraganglioma. He was subsequently found to have an associated genetic syndrome. This is the first case report describing a primary pulmonary paraganglioma in a child.
INTRODUCTION
Paraganglioma is a rare extra-adrenal tumors of the paraganglia often found in association with sympathetic and parasympathetic nerves. Primary pulmonary paragangliomas are rare and per an extensive review of the literature, this is the first case report that describes a primary pulmonary paraganglioma in a pediatric patient.
CASE REPORT
Presentation
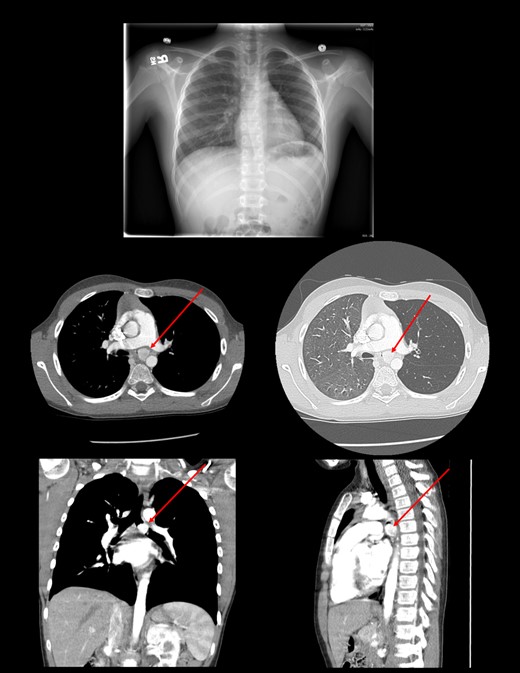
The patient is a 10-year-old boy who presented to an emergency room with hemoptysis. Work-up showed normal laboratory findings and negative Quantiferon gold. Radiography of the chest showed hyperinflation on the left lung. Subsequent CT scan of the chest showed a 1.7 cm hypervascular mass in the proximal left main-stem bronchus.
Medical history included allergic rhinitis, pneumonia at ages 2 and 8 treated with oral antibiotics, and asthma, for which he was on maintenance therapy with fluticasone-salmeterol. Symptoms had worsened in recent months with audible wheezing that was non-responsive to albuterol treatments. His review of systems was otherwise negative.
His physical exam was significant for decreased air movement over the anterior left chest with high pitched inspiratory and expiratory wheeze on auscultation.
Diagnosis
Laboratory findings showed a normal C-reactive protein, erythrocyte sedimentation rate and white blood cell count.
Chest radiography showed dilation of the proximal left main-stem bronchus with focal truncation distally. Review of his chest CT confirmed a large hypervascular mass in the left main-stem bronchus (Fig. 1).
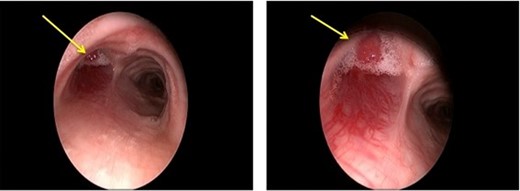
Rigid bronchoscopy was performed, confirming an intraluminal hypervascular mass occluding the entire left main-stem bronchus with visible vasculature extending into the posterior tracheal wall. The mass had a smooth appearance with telangiectasias and extensive friability (Fig. 2). A biopsy of the mass suggested an atypical neuro-endocrine tumor.
TREATMENT
The patient was taken to the operating room and bronchoscopy confirmed a nearly completely obstructing mass of the proximal left main-stem bronchus without invasion of the mass into the carina. A video-assisted left thoracoscopy showed that the mass was growing through the bronchus, but not invading surrounding structures. There was inflammation in the surrounding bronchus. Lymph nodes in the subcarinal region did not appear grossly malignant. There was no pleural studding or effusion and the remainder of the lung was found to be normal. We then performed a serratus-sparing posterior thoracotomy in the fourth intercostal space to biopsy and resect the mass. We performed a left main-stem bronchus sleeve resection by transecting proximal and distal to the external mass. This tissue was sent for frozen section. Initial pathology showed neoplasm, likely neuro-endocrine tumor. Margins on the frozen specimen were negative. Lymph nodes from stations 7, 4 L and 11 L were sent for permanent pathology. The two ends of the bronchus were re-anastomosed using a series of interrupted 5-0 PDS sutures for the membranous bronchus and interrupted 4-0 Vicryl sutures for the cartilaginous portion. Bronchoscopy confirmed patent anastomosis without twisting of bronchus. There was a good size match between carina and distal left main-stem bronchial ends. A pedicled intercostal muscle flap, which was harvested on chest entry, was loosely wrapped around the anastomosis. He was extubated at the conclusion of the case.
Post-operatively, the patient recovered in the Pediatric Intensive Care Unit and had an uncomplicated course. The chest tubes were removed on post-operative Day 5. He was discharged 7 days post-operatively.
PATHOLOGY
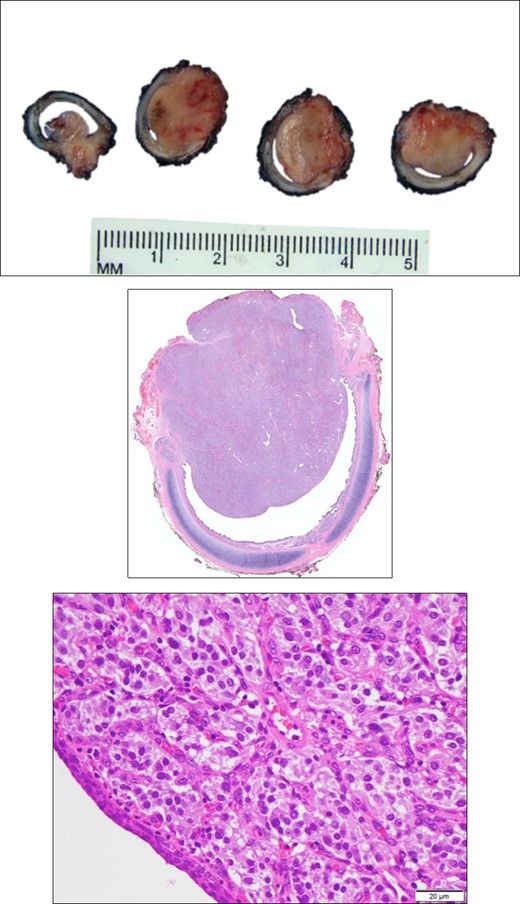
Sections of the mass showed a cellular tumor surrounded by a thin band of fibrous tissue in a trabecular pattern. The majority of tumor cells were chief cells with medium sized round nuclei with granular chromatin, small nucleoli and ample granular eosinophilic cytoplasm. There was strongly positive staining for S-100, synaptophysin and CD56. Cytokeratin staining was negative. These findings are consistent with paraganglioma (Fig. 3).
FOLLOW-UP AND OUTCOME
At follow-up, 2 weeks post-operatively, the patient had no exercise intolerance or wheezing. A chest MRI 9 months post-operative showed no evidence of recurrent tumor and a patent airway without intraluminal lesions or airway mass effect. The patient has fully recovered from his resection without complication and remains active without airway symptoms. Our patient and his father were found to have a mutation in the SDHA gene.
COMMENT
Airway pathology in children is common. Etiologies include foreign bodies, structural abnormalities such as subglottic stenosis, tracheomalacia, laryngomalacia, infectious or inflammatory processes, and neoplasms [1]. Compared to adults, infants and children are more likely to become symptomatic from airway lesions due to smaller airway caliber and collapsibility. Pulmonary neoplasms are overall rare in children and the differential diagnosis includes: primary tracheobronchial tumors (carcinoid, neuro-endocrine), hemangioma, lymphoma, sarcoma and metastatic disease. Metastatic tumors are more common than primary lung neoplasm with a ratio of 3 to 1 [2].
Paragangliomas are rare neuro-endocrine tumors derived from extra-adrenal autonomic paraganglia. First described in 1958, they are closely related to pheochromocytomas and have the ability to secrete catecholamines [3]. Paragangliomas in children are usually linked to a hereditary syndrome. Hereditary paragangliomas occur more often at a younger age and are associated with syndromes with an autosomal dominant inheritance pattern including MEN 2A or 2B, Von Hippel Lindau and neurofibromatosis. Familial paragangliomas are usually seen in the SDH complex genes (SDHA, SDHB, SDHC and SDHD) which are involved in the energy metabolism of the cell [4]. Primary pulmonary paragangliomas are parasympathetic and are mostly found associated with pulmonary nerves and vessels [5].
The diagnosis of a primary pulmonary paraganglioma is made through a combination of plasma metanephrines/urinary catecholamines, radiology and biopsy. Histologically, paragangliomas demonstrate epithelioid cell nests surrounded by vascular tissue and sustentacular cells (Zellballen pattern) which stain for S-100 protein. There is an absence of carcinoid architecture and they rarely stain for cytokeratin [5].
For this patient, diagnosis was not made until symptoms worsened, but fortunately his tumor had not spread. We were able to achieve a complete left lung-sparing sleeve resection of the left main-stem bronchus with negative margins and no evidence of recurrent disease at 9 months.
Based on these findings and known pathogenesis, genetic testing (PGLNext panel) should be offered to all pediatric cases of paraganglioma to identify risk of other malignancy. Surgery with intent to cure this tumor is both safe and effective.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest relevant to this article to disclose.
FUNDING
The authors have no financial relationships relevant to this article to disclose
CLINICAL TRIAL REGISTRATION
Not applicable.
PRESENTATIONS
American Thoracic Society Annual Meeting 2017: Poster presentation, a case report of a 10-year-old boy with paraganglioma.
TABLE OF CONTENTS SUMMARY
This is a case report of pediatric patient with a primary pulmonary paraganglioma. It includes a review of the literature and a description of the bronchial sleeve resection used for treatment.
CONTRIBUTORS STATEMENT
Drs Geoffrion, DeKeyser, Nair and Pirolli conceptualized and designed the study, collected data, drafted the initial manuscript and reviewed and revised the manuscript. Drs Shah, Nair and Kernstine critically reviewed the manuscript for important intellectual content and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.



