-
PDF
- Split View
-
Views
-
Cite
Cite
Emily Higgins, Liam Monaghan, Raghu R. Mani, Cutaneous metastasis of a primary oesophageal adenocarcinoma to the right cheek, Journal of Surgical Case Reports, Volume 2017, Issue 9, September 2017, rjx181, https://doi.org/10.1093/jscr/rjx181
Close - Share Icon Share
Abstract
This case report details of a case of cutaneous metastasis from a primary adenocarcinoma of the oesophagus to the right cheek. A 67-year-old male was referred to the maxillofacial department with a 2–3 week history of non-painful swelling of the cheek. A diagnosis of infected sebaceous cyst was made and drainage was attempted with adjunctive antibiotic therapy. Follow up appointments showed no improvement a biopsy was taken. Histology reported presence of metastatic adenocarcinoma, suggesting the gastrointestinal tract as the primary site. An MRI scan was performed showing an oesophageal mass. Treatment options were discussed with the patient, including surgery, radiotherapy and chemotherapy. Unfortunately, the advanced nature of the primary lesion meant his care was mainly palliative in nature. Clinicians must have a high index of suspicion regarding non-healing cutaneous lesions. Timely investigations in the will help to diagnose the primary cause of the lesion.
INTRODUCTION
Oesophageal cancer is relatively common, with a lifetime risk of 1 in 55 for males and 1 in 115 for females in the UK [1]. Metastatic disease is most commonly reported in the liver, lungs, adrenal glands and bones [2]. Cutaneous metastatic lesions are exceedingly rare, with few cases reported in the literature. Diagnosis can be difficult and lesions may be mistaken for other cutaneous conditions.
CASE REPORT
A 67-year-old male was referred to the Maxillofacial Unit after presenting to the Emergency Department with a facial swelling. Medically, the patient was fit and well, with a history of smoking 20 cigarettes per day and 20 units of alcohol per week. There was a soft, erythematous swelling of the right cheek measuring 3 × 3 cm. It was painful, without a discharging punctum and had features of an infected sebaceous cyst. The patient was not complaining of dysphagia and was systemically well. Intra-oral examination showed chronic periodontal disease and carious teeth but no sign of acute infection (Figs 1 and 2).

Image showing the indurated, exophytic tumour following incisional biopsy. Source: Royal Albert Edward Infirmary.
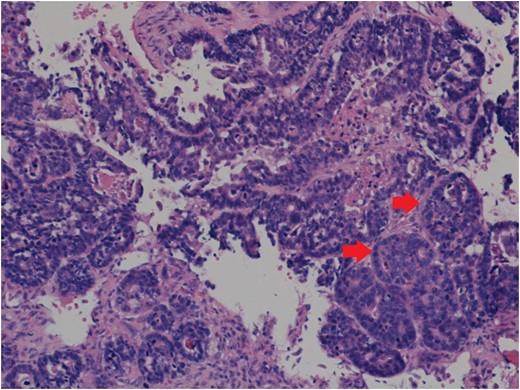
Histology showing paraspinal tissue replaced and permeated by metastatic adenocarcinoma with large areas of necrosis. Arrows point to clusters of tumour cells. Source: Salford Royal Hospital Histology Department.
A diagnosis of an infected sebaceous cyst was formulated and arrangements made for incision and drainage under local anaesthesia. Unfortunately, the patient then left the department before treatment was undertaken. He returned 1-week later with the same complaint, when the lesion was drained and a review appointment made. A review at 1 week found the erythematous area to have increased in size, with the incision site now having an exophytic, indurated appearance. An urgent biopsy was undertaken and ultrasound scan arranged.
Histology showed a high grade adenocarcinoma with appearances unlikely to represent a primary adnexal carcinoma. The immunoprofile of the specimen suggested a metastatic deposit of a tumour originating in the gastrointestinal tract or pancreatico-biliary system. In light of this, a CT abdomen, thorax and pelvis was undertaken whilst a referral was made to a gastrointestinal surgeon. CT showed a large tumour of the lower oesophagus with multiple metastatic lymph nodes, bony metastasis in vertebrae L2 and lung metastases. Oesophageal biopsies confirmed an invasive adenocarcinoma, just superior to the gastro-oesophageal junction. Spinal decompression and stabilization was undertaken, in order to maintain quality of life, and he was discussed at the UGI MDT where it was decided that treatment would be palliative in nature. Radiotherapy involved five fractions to the lumbar spine and right cheek, before referral to a medical oncologist for palliative chemotherapy. The cheek mass had responded well to radiotherapy and the patient was placed on a course of epirubicin, oxaliplatin and capecitabine (Xeloda, Manufacturer Hoffman La Roche) for the oesophageal tumour. On review, a CT scan showed progression of bony disease and lung metastases along with a collapse of C4, and at this point the oncologist estimated survival to be that of 3–6 months. The patient died soon after.
DISCUSSION
Adenocarcinoma is the most common oesophageal cancer in the western world, whilst squamous cell carcinoma remains more prevalent in developing nations [3]. Both types share common risk factors of tobacco and alcohol use, and a diet low in fruit and vegetables. Adenocarcinoma is strongly associated with gastro-oesophageal reflux and Barrett’s oesophagus [4].
Metastatic deposits of these cancers are mostly seen in the liver, lungs and bones [2]. Cutaneous metastasis remain rare, with most reported cases involving squamous cell tumours [5, 6]. Metastatic lesions have been recorded as presenting on the skin of the limbs, back and abdominal wall [5, 7, 8]. Lesions in the head and neck have presented in the skin of the lip, frontal and temporal regions and the scalp [5, 9, 10]. The incidence of oesophageal carcinoma is rising [4], and it has been proposed that this, alongside improvements in management could lead to cutaneous metastasis becoming more common.
Oesophageal carcinomas are frequently diagnosed at a late stage, often presenting as dysphagia and weight loss, although skin lesions can be the presenting symptom in advanced disease. Our patient showed no concerning features or signs of systemic illness. He had no prior history of gastro-oesophageal reflux or dysphagia, and the only sign of underlying neoplasia was the facial lesion. Most commonly, cutaneous metastases present as solitary, fixed, painless nodules. However, lesions can have varied appearances, including multiple papules; friable, bleeding masses; and in our case a soft erythematous swelling [7, 5, 6, 10]. With such diverse presentations, these lesions can be misdiagnosed, leaving them ignored, or initially managed with topical dermatological ointments [7] . In the case described, the clinical appearance mimicked that of an infected sebaceous cyst, with sinister features such as induration and exophytic growth not appearing until after the biopsy. This highlights the difficulty in diagnosing lesions clinically, and histopathalogical conformation should be sought at the earliest opportunity, should apparently benign lesions persist.
Clinicians must treat lesions that do not respond to conventional treatment with suspicion. In this case, the diagnosis of sebaceous cyst was consistent with the initial presentation of the lesion. However, the indurated, exophytic healing at the site of the biopsy was a red flag symptom of malignancy. Timely diagnosis of lesions will help to uncover any causative underlying conditions, and will allow for appropriate treatment to increase patient survival and improve outcomes.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- magnetic resonance imaging
- radiation therapy
- edema
- biopsy
- chemotherapy regimen
- esophageal adenocarcinoma
- cheek
- epithelial cyst
- esophageal neoplasms
- follow-up
- pain
- surgical procedures, operative
- diagnosis
- histology
- palliative care
- surgery specialty
- skin lesion
- antibiotic therapy
- gastrointestinal tract
- secondary malignant neoplasm of skin
- adenocarcinoma, metastatic



