-
PDF
- Split View
-
Views
-
Cite
Cite
Edward Holloway, Paul Sutton, Robert Cooper, An unusual cause of genu valgum and persistent instability, Journal of Surgical Case Reports, Volume 2017, Issue 8, August 2017, rjx166, https://doi.org/10.1093/jscr/rjx166
Close - Share Icon Share
Abstract
We present the case of a professional adolescent footballer who attended our clinic with ongoing instability symptoms and valgus knee deformity after conservative management of an medial collateral ligament injury. The patient was found to have sustained a contra-coup Salter Harris Type V injury to his lateral distal femur physis resulting in premature growth arrest and deformity. Salter Harris Type V injuries are rare, and often not diagnosed until growth has arrest has occurred due to lack of identifiable features on initial plain radiographs. The patient was successfully treated with opening wedge femoral osteotomy and plication of the medial collateral ligament. This case reinforces the need for awareness of such injuries to avoid delayed diagnosis and describes options for management.
INTRODUCTION
The medial collateral ligament (MCL) is one of the most commonly injured ligaments in the knee. Injury usually follows a valgus insult. Injuries are graded I–III according to the degree of joint laxity on application of a valgus stress during clinical examination. Most injuries can be successfully managed conservatively with bracing alone.
Salter Harris Type V injuries are uncommon and rarely reported as causing knee deformity. They have been reported in the proximal tibia as resulting in recurvatum of the knee [1], but have not, as far as we are aware, been reported in the distal femur as presenting with genu valgum in association with MCL injury.
The purpose of this case report is to present the unusual example of an adolescent patient presenting with ongoing instability following a conservatively managed MCL injury which was found to be associated with a previously missed contra-coup lateral distal femoral Salter Harris Type V injury and consequent growth disturbance. This case discusses the need to be vigilant for such injuries in the immature skeleton, the difficulties of diagnosis, and options for management.
CASE REPORT
A 16-year-old elite level footballer presented to our clinic with persistent symptoms of instability following a knee injury. The patient had sustained a valgus force to his knee during a tackle. He had been treated by his football club's doctor after an magnetic resonance imaging (MRI) scan had demonstrated a MCL injury (Fig. 1).

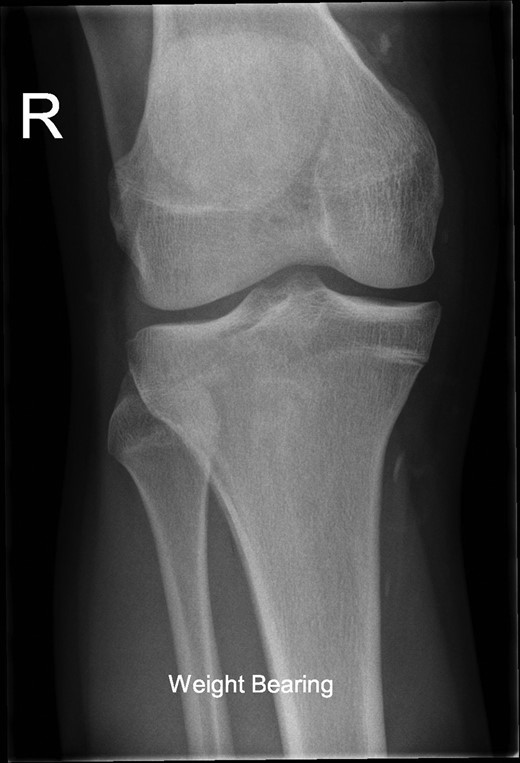
The patient's initial management was non-operative with a period of knee protection with a range of movement brace and intensive rehabilitation. Approximately 3 months after the index injury he returned to competitive football but shortly after his return sustained a further valgus injury and despite further conservative treatment was unable to return to sport. He was referred to our service with ongoing instability symptoms. Upon clinical assessment we noted an asymmetric valgus alignment of the knee and abnormal laxity of the MCL. Radiographic investigations revealed an abnormality of the lateral distal femur and alignment radiographs confirmed the valgus mal-alignment with abnormal opening of the medial tibio-femoral joint space on single-leg stance radiographs (Figs 2–4). We obtained the patient's MRI scan and reviewing this with Radiology colleagues revealed subtle changes of increased lateral femoral physis fluid density on T-2 weighted images consistent with a Salter Harris Type V injury (Fig. 5).

Long-leg alignment radiograph showing valgus deformity of the right knee.

Radiograph demonstrating opening of the medial compartment and increased valgus alignment on single-limb weight bearing.

MRI showing increased fluid density around the lateral distal femoral physis (red arrow).
We believe that the patients index MCL injury was complicated by a contra-coup Salter Harris Type V injury, resulting in premature closure of the lateral portion of the distal femoral physis. We concluded that the resultant valgus deformity combined with residual laxity of the MCL were responsible for the patient's symptoms of instability.
The patient was counseled as to the nature of their injury and the likelihood of ongoing instability and potential for early degenerative change with conservative management. The deformity and instability were successfully treated with an opening distal femoral osteotomy combined with surgical plication of the MCL (Figs 6 and 7). At the time of reporting, 2 years following surgery, the patient has successfully returned to playing competitive football without symptoms of instability. The metalwork remains in situ.


DISCUSSION
The distal femoral physis contributes 70% of the total femoral growth, on average 1.2 cm per year, increasing to 1.4 cm per year at puberty [2]. Susceptibilty to injury is the greatest around the time of maximal growth.
Distal femoral physis fractures account for ~5% of Salter Harris injuries. They are prone to complications including a significant risk of permanent injury to the physis with resultant growth disturbance [3]. Type V injuries comprise a very small proportion of distal femoral SH fractures [4]. When a valgus force is applied to the immature knee, the cartilaginous matrix of the physis on the tension side is more vulnerable to distraction, whereas on the compression side, the osseous metaphysis is more vulnerable to shear failure from compression. As a result, Salter Harris Types I and II injuries with the Thurston-Holland fragment on the lateral side of the knee are most commonly seen.
A Salter Harris Type V injury was originally described as a ‘very severe crushing force applied through the epiphysis to one area of the epiphyseal plate’ [5]. The precise mechanism of physeal damage is probably a combination of microscopic disruption and splitting as well as vascular disruption [6]. It occurs without an associated epiphyseal or metaphyseal fracture and is therefore difficult to diagnose on initial radiographs. Frequently, the diagnosis is only made retrospectively when the patient presents with premature closure of the physis and disturbance of growth [7, 8].
A well described surgical technique for the treatment of instability arising from a lateral collateral ligament or postero-lateral corner injury in the presence of a constitutional varus deformity is correction of limb alignment. This procedure is performed in order to protect a soft tissue repair or ligament reconstruction which has been demonstrated to be associated with less satisfactory outcomes if performed without addressing varus mal-alignment [9]. The procedure is usually performed prior to the ligament reconstruction, however, following limb re-alignment ligament reconstruction is not always required.
Although the management of lateral instability in the presence of a varus lower limb alignment is well described and understood, managing medial instability in the presence of a valgus deformity is less commonly reported [10]. Using the principles we employ when managing a lateral sided injury with varus deformity we treated this unusual problem by correction of the abnormal alignment and simultaneous repair of the ligamentous injury with a satisfactory functional outcome.
The patient had a opening wedge osteotomy performed using the technique described by Puddu et al. [11]. Alternative options to correct the deformity would have been a closing wedge medial tibial osteotomy or use of an Ilizarov-type external fixation. Medial proximal closing wedge tibial osteotomies heal well without the need for graft but result in loss of height [12]. Ilizarov devices allow reliable early weight bearing and have the benefit of not leaving metalwork in situ but are not always well tolerated or accepted by patients [13].
We recognize that Salter Harris V injuries of the distal physis are rare and difficult to diagnose but advise that this injury is considered in any skeletally immature patient following a significant knee ligament injury. Further investigations to be considered are radiographs of the contra-lateral limb allowing comparison of the shape and thickness of the physes and MRI to exclude intra-osseous effusion, periosteal reaction or occult fractures [14].
CONFLICT OF INTEREST STATEMENT
None declared.



