-
PDF
- Split View
-
Views
-
Cite
Cite
Georgios Sahsamanis, Georgios Mitsopoulos, Titos Deverakis, Alexandra Terzoglou, Paschalis Evangelidis, Georgios Dimitrakopoulos, Neuroendocrine carcinoma as a rare cause of jejunal intussusception in an adult. Management and literature review, Journal of Surgical Case Reports, Volume 2017, Issue 5, May 2017, rjx082, https://doi.org/10.1093/jscr/rjx082
Close - Share Icon Share
Abstract
Intussusception of the small bowel is an uncommon condition, with the majority of cases being observed during infancy. A number of points are responsible, with benign and malignant lesions of the small intestine being the most common. Herein, we present the case of a 75-year-old male patient with vague abdominal pain and black stool during defecation, who underwent surgery due to jejunal intussusception. Pathology report demonstrated a neuroendocrine carcinoma as the underlying cause for his condition, with no additional metastases during the initial diagnosis. Although a conservative approach for management of intussusception is viable, the possibility of gastric outlet obstruction and the presence of malignancy as the primary point usually lead to urgent surgery. In the case of malignancy, adjuvant chemotherapy or additional symptomatic therapy with close follow-up may be required depending on tumor’s grade and aggressiveness.
INTRODUCTION
Small bowel intussusception is a rare condition in adulthood, with benign and malignant gastrointestinal lesions being the main causative points. The possibility of gastric outlet obstruction and advanced malignant disease often indicate for an urgent surgical treatment. We present the case of a 75-year-old male who suffered from small bowel intussusception due to a neuroendocrine carcinoma (NEC). We will also review the literature regarding management of both medical conditions and their relation.
CASE REPORT
A 75-year-old Caucasian male was referred to our department due to black stool during defecation and episodes of cramp-like abdominal pain for the past 2 months. His medical history included hypertension and chronic obstructive pulmonary disease (COPD), while he also reported treatment for a peptic ulcer at the age of 40 and appendectomy at a younger age. Physical examination was insignificant, with digital rectal examination being negative. Laboratory exams revealed a hematocrit of 28.4 mg/dl with hemoglobin of 8.4 mg/dl. Rest of the biochemistry exams where within normal limits.
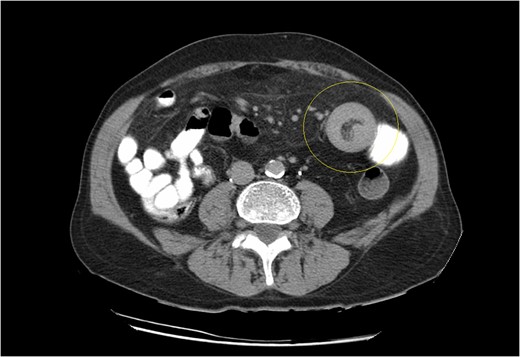
CT scan demonstrating the typical ‘doughnut’ sign of bowel intussusception.
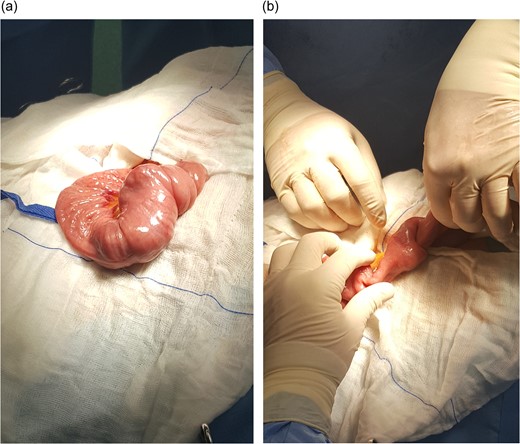
(a, b) Small bowel intussusception located in the proximal jejunum.
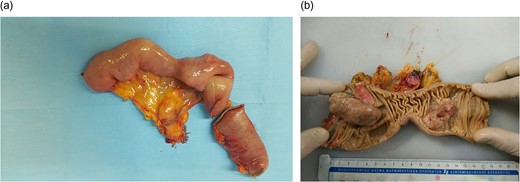
(a, b) Excised specimen demonstrating two NECs responsible for the intussusception.
Pathology report demonstrated two large cell, low differentiated, stage IIIB according to ENETS, NECs of the jejunum (pT3N1a). Immunohistochemical report was positive for synaptophysine and chromogranin A (CgA), as well as Ki-67 proliferative activity.
Patient tolerated surgery well, with normal intestinal function on the second postoperative day. He was discharged on the fourth postoperative day, with a hematocrit of 31.2 mg/dl. He started adjuvant chemotherapy with somatostatin analogues (SSA), while at 6-month follow-up no metastases were observed.
DISCUSSION
Small bowel intussusception is defined as the distal protrusion of a small bowel loop (intussusceptum) inside the lumen of an adjacent bowel segment (intussuscipiens) along with its mesentery [1]. It is a rare medical condition in the general population with the vast majority of cases (95%) being observed during the first trimester of infancy. In adulthood, intussusception is encountered in ~2% of gastric outlet obstruction cases [1, 2]. It is classified according to etiology to benign, malignant and idiopathic, with metastatic tumors (melanoma, lung cancer and breast cancer) and gastrointestinal malignancies or benign neoplasms (polyps) being the leading points [3].
Clinical manifestation is often obscure with symptoms being associated with partial or complete bowel obstruction. Vague abdominal pain, nausea or episodes of vomitting are usually observed, while patients can also exhibit episodes of abdominal distension and ileus. Abdominal cramp-like pain, or constipation and weight loss may also be present, suspicious for an underlying malignant pathology [3, 4].
Computed tomography is the modality of choice for diagnosis of an intussuscepted bowel loop, with a sensitivity and specificity of ~80% and 100%, respectively. Depending on sagittal or axial view, findings may include the presence of concentric rings due to duplication of small bowel layers (‘doughnut’ or ‘target’ sign), or a sausage shaped mass [3, 5, 6]. U/S scan is also useful for identification of intussuscepted bowel with the typical ‘target sign’ [6]. Diagnosis is usually set intraoperatively, because of the nonspecific clinical symptoms and non-pathognomonic radiological findings.
Treatment can be either conservative, in cases which no evident pathology is present, or surgical excision of the pathologic bowel part through open or laparoscopic surgery. Since malignancies are the primary cause for most intussusception cases, most surgeons agree to a surgical approach, with ~60% of interventions being executed in an emergency setting [1, 3]. Reduction of the small bowel in order to avoid surgery and save bowel length is dangerous due to the possibility of bowel perforation and migration of malignant cells [7].
Neuroendocrine neoplasms (NENs) of the small intestine are rarely associated with intussusception in the medical literature. Up to 10% of patients may exhibit symptoms typical of carcinoid syndrome consisting of (i) skin flushing, (ii) diarrhea or cramp-like abdominal pain and (iii) musculoskeletal symptoms. NECs consist a rare subtype of NENs with a particularly aggressive behavior [8]. Treatment of NECs involves their complete surgical resection within healthy tissue. Adjuvant therapy with SSA is recommended, markedly improving patients’ quality of life, with a significant reduction of carcinoid syndrome symptoms in up to 75% of cases. Chemotherapy is a contradiction in cases of well-differentiated or metastatic neoplasms, while patient’s follow-up includes CT scan every 3–12 months and control of CgA and 5-hydroxyindoleacetic acid levels [8].
In a recent publication, Kadowaki et al. [9] presented a case of gastroduodenal intussusception due to a collision tumor, consisting of adenocarcinoma and a NEC. In another report, Lachhab et al. [10] described the case of a patient with small bowel intussusception due to a neuroendocrine tumor. In the first case, patient underwent surgical resection with no adjuvant chemotherapy and metastatic hepatic and splenic tumors after 6 months, while in the second case patient underwent excision of the intussuscepted bowel loop with no further therapy, and no metastases reported at 6-month follow-up [9, 10].
In conclusion, although NECs and intussusception of the small intestine are rarely associated, the tumor’s aggressiveness and possibility of complete gastric outlet obstruction suggest for an aggressive therapeutic approach with close follow-up monitoring.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and corresponding images.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
Nothing to declare.



