-
PDF
- Split View
-
Views
-
Cite
Cite
Austin R. Dosch, Madeleine Pahl, Uttam Reddy, Clarence E. Foster, Hirohito Ichii, Post-transplantation nephroptosis causing recurrent episodes of acute renal failure and hypertension secondary to intermittent vascular torsion of intraperitoneal renal allograft, Journal of Surgical Case Reports, Volume 2017, Issue 5, May 2017, rjx033, https://doi.org/10.1093/jscr/rjx033
Close - Share Icon Share
Abstract
Nephroptosis is a rare complication in renal transplantation, but one with significant associated risk. Due to non-specific clinical features, there may be a substantial delay in diagnosis and loss of the transplanted kidney due to renal pedicle thrombosis. We present a case of post-transplantation nephroptosis after simultaneous pancreas and kidney transplant, which resulted in accelerated hypertension and reversible acute kidney injury >1 year after transplantation. Prompt detection of this rare entity leading to expeditious surgical intervention is necessary to preserve viability of the renal allograft.
INTRODUCTION
Traditionally, Nephroptosis has been referred to as ‘floating kidney syndrome’. This was thought to be due to congenital deficiency of Gerota's fascia allowing for excessive, retro-peritoneal renal mobility. Severe complications can result including ureteral obstruction, intermittent vascular occlusion or traction of hilar nerves causing flank pain. Episodic hypertension can develop due to activation of the renin–angiotension–aldosterone axis that occurs with reduced renal blood flow from intermittent arterial occlusion. Symptomatic patients are treated with nephropexy that prevents free rotation of the kidney around its fixed vascular pedicle. While this phenomenon is well-described in the general population, there are few reports of nephroptosis in renal transplantation. Renal allografts are typically transplanted in the iliac fossa which limits potential for migration, although intra-abdominal transplantation is performed in simultaneous kidney-pancreas transplant (SPK) or dual renal transplantation. Most patients develop sufficient intra-abdominal scar tissue so allograft mobility is restricted; however, this does not always occur. We present a case report with pathologic post-transplantation nephroptosis after SPK successfully treated with nephropexy.
CASE PRESENTATION
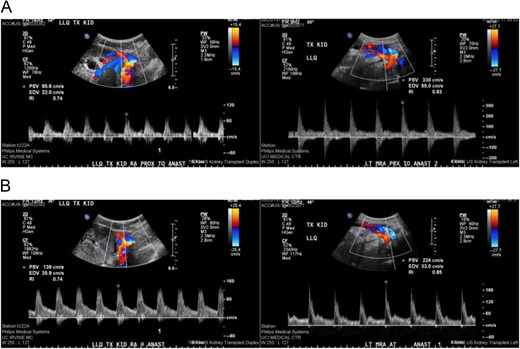
Comparison of duplex ultrasound of transplanted kidney in August 2015 compared to September 2015. Elevated velocities proximal and at the main renal artery anastomosis to 330 cm/s from 85.6 cm proximal to anastomosis (A) and 224 cm/s from 139 cm/s at the site of the anastomosis (B).

Comparison of CT scans obtained July 2015 (A) and August 2015 (B) showing migration of the transplanted renal allograft within the peritoneal cavity.
DISCUSSION
Nephroptosis in a transplanted renal allograft is an uncommon occurrence. When complete torsion of the renal axis occurs, AKI can develop and be easily confused with more common causes of acute renal failure such as rejection or obstruction. This can delay diagnosis and lead to irreversible allograft damage secondary to prolonged ischemia. A high index of suspicion is necessary to facilitate diagnosis of this rare phenomenon. Intraperitoneal renal transplant places the allograft into a larger compartment than the iliac fossa, which may predispose patients to developing post-transplantation nephroptosis [1]. In addition, patients receiving sirolimus have been shown to have impaired wound healing and presumably are also deficient in inflammatory cytokines necessary to form intra-abdominal adhesions, allowing free rotation to occur [2].
Presenting symptoms of nephroptosis most commonly include AKI, abdominal pain, decreased urine output and nausea/vomiting [3]. Doppler studies may reveal elevated flow velocities or complete occlusion of the vascular pedicle, but may also be normal if there is no active torsion of the renal allograft. Most common changes seen in a single study were shown to be reversed arterial diastolic flow, often with vascular thrombosis [1]. Identifying positional variations in renal blood flow may also be useful, although this has not been extensively studied. Sequential CT scans may also demonstrate migration of the renal allograft or change in axis, as was the case described above and has been reported previously as well [4].
Prophylactic suture nephropexy may be undertaken at the time of transplantation to reduce the risk of post-operative nephroptosis [3]. We now routinely perform this during intra-abdominal renal transplants at our institution.
Post-transplant nephroptosis is a rare but potentially severe complication of intraperitoneal kidney transplant that can be successfully managed with appropriate surgical intervention [5]. It should be suspected in all patients with acute vascular compromise or recurrent episodes of renal failure without discernable cause. Transplant surgeons and nephrologists should be familiar with this unusual but surgically manageable cause of AKI.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- thrombosis
- renal transplantation
- malignant hypertension
- hypertension, secondary
- renal failure, acute
- signs and symptoms
- surgical procedures, operative
- kidney
- transplantation
- renal pedicle
- renal and pancreas transplantation
- nephroptosis
- intraperitoneal infusion
- transplanted kidney
- allografting
- delayed diagnosis



