-
PDF
- Split View
-
Views
-
Cite
Cite
Tomohiro Haruki, Makoto Wakahara, Yuji Taniguchi, Yoshinobu Nakamura, Motonobu Nishimura, Hiroshige Nakamura, Successful multimodality treatment for locally advanced primary thymic adenocarcinoma: report of a case, Journal of Surgical Case Reports, Volume 2016, Issue 8, August 2016, rjw148, https://doi.org/10.1093/jscr/rjw148
Close - Share Icon Share
Abstract
Although the optimal treatment strategy for locally advanced thymic carcinomas has yet to be determined, complete resection of the tumor after induction chemoradiotherapy (CRT) can sometimes provide a good chance of being cured. A 61-year-old woman was diagnosed with locally advanced primary thymic carcinoma, which invaded bilateral brachiocephalic veins and superior vena cava with intraluminal tumor thrombus. Induction CRT was performed, and a partial response to the treatment was achieved. Subsequent radical surgery was successfully performed by the median full sternotomy with a right transmanubrial osteomuscular sparing approach (TMA). The patient is currently alive and has remained disease-free for a year. The TMA is useful for extensive surgery of locally advanced thymic carcinoma because it can provide good exposure of the operative field without post-operative functional limitation of upper limbs.
Introduction
A recent treatment trend of locally advanced thymic tumors seems to be induction chemoradiotherapy (CRT) followed by surgery because several recent clinical trials had revealed that the addition of preoperative therapy before resection for them might enhance the ability to perform complete resection with acceptable toxicity [1]. Even if therapeutic effects of preoperative therapies are obtained, complete resection of the tumor is a pivotal treatment and essential for favorable outcomes of locally advanced thymic tumors [2]. Surgical approaches are crucially important to perform more sophisticated operations, especially around the cervicothoracic region. Transmanubrial osteomuscular sparing approach (TMA) is one of these approaches and allows excellent unilateral exposure of the thoracic outlet.
We report a case of locally advanced primary thymic adenocarcinoma with a successful multimodality therapy including an extended radical surgery performed by TMA with median sternotomy.
Case Report
A 61-year-old woman was admitted to our hospital with edema of both upper limbs and face. Blood examination results were almost normal, but, carcinoembryonic antigen was slightly elevated (7.1 ng/ml). A chest X-ray on admission showed an enlarged superior mediastinum and right diaphragmatic elevation (Fig. 1). Enhanced computed tomography (CT) of the chest showed an invasive anterior mediastinal tumor, 6.0 × 3.7 cm in size, invading to bilateral brachiocephalic veins and superior vena cava (SVC) with intraluminal tumor thrombus (Fig. 2a–c). Percutaneous CT-guided biopsy of the tumor was performed immediately after admission, and this tumor was diagnosed as adenocarcinoma, with the suspicion of primary thymic carcinoma or metastatic thymic tumor from gastrointestinal malignancies (Fig. 3a,b). Immunohistochemical examination showed that the tumor cells were positive for cytokeratin 20 and caudal type homeobox 2. Systemic workups revealed no other primary sites or any distant metastases, and she was finally diagnosed as having locally advanced primary thymic adenocarcinoma. Induction CRT was provided to induce a reduction of the tumor with the aim of complete resection. She was administered chemotherapy consisting of carboplatin and paclitaxel on a weekly basis and was treated concurrently with thoracic radiotherapy (50 Gy; 2.0 Gy × 25 fractions). The chest CT after induction CRT demonstrated a reduction of the tumor (partial response: 43% reduction in tumor diameter) and improvement of venous tumor thrombus (Fig. 2d–f). During the CRT, symptomatic SVC syndrome gradually improved, and no severe acute toxicity was observed.
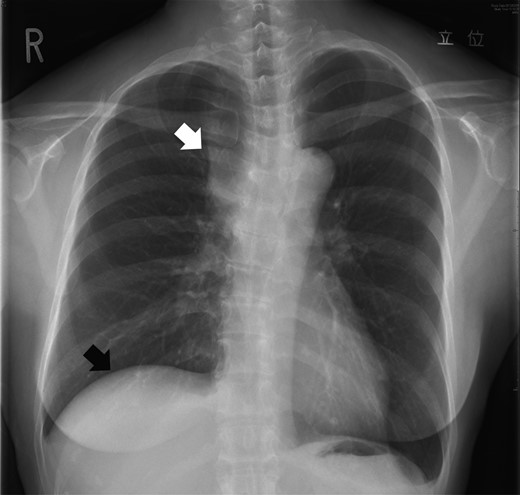
A chest X-ray on admission showed an enlarged superior mediastinum (white arrow) and right diaphragmatic elevation (black arrow).
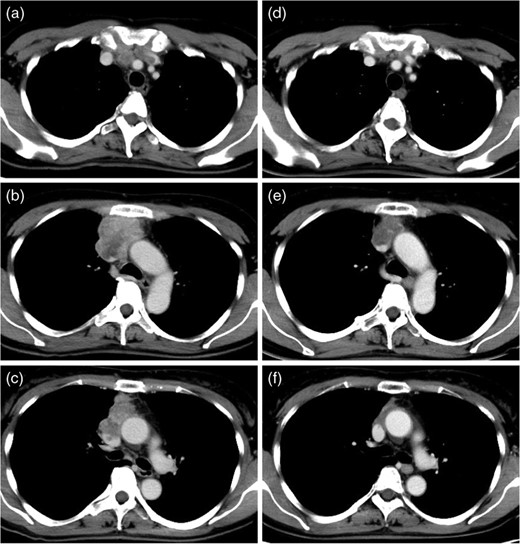
Preoperative enhanced CT of the chest (a, b, c) showed an invasive anterior mediastinal tumor, extending to bilateral brachiocephalic veins and SVC with intraluminal tumor thrombus. After induction CRT, the mediastinal tumor was shrunk and intraluminal tumor thrombus of great veins was improved (d, e, f).
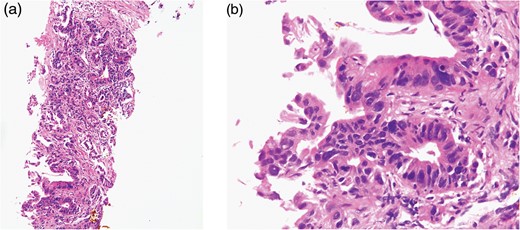
The tumor was diagnosed as thymic adenocarcinoma with enteric differentiation, with the suspicion of primary thymic carcinoma or metastatic thymic tumor from grastrointestinal cancer (a: HE stain × 40; b: HE stain × 100).
Subsequently, curative-intent surgery was scheduled. It was thought that extended thymothymectomy with combined resection of bilateral brachiocephalic veins and SVC was needed to resect the tumor completely. To obtain good exposure of the operative field, we selected median full sternotomy with right TMA (Fig. 4a). The tumor was resected along with part of the pericardium, part of the right upper lobe of the lung, bilateral brachiocephalic veins, azygos vein, right phrenic nerve and SVC because of the tumor invasion (Fig. 4b). Before the combined resection and reconstruction of SVC, a temporal veno-venous bypass between right internal jugular vein and right atrial appendage was established (Fig. 4c). SVC reconstruction was performed by end-to-end anastomosis of a ringed polytetrafluoroethylene graft (10 mm in diameter) between residual right brachiocephalic vein and SVC using a running parachute technique with a 5-0 prolene suture (Fig. 4d). The operation was finished with no trouble and complete radical resection of the tumor was achieved. The operating time was 441 minutes and blood loss was 880 ml. Histological examination of the surgical specimen showed a few residual viable tumor cells in extensive fibrous scarring lesion with hyalinization. Adjuvant chemotherapy was not provided, and she received post-operative anticoagulation therapy with warfarin (3.0 mg/day) and low-dose aspirin (100 mg/day), and remained disease-free for 12 months after operation.
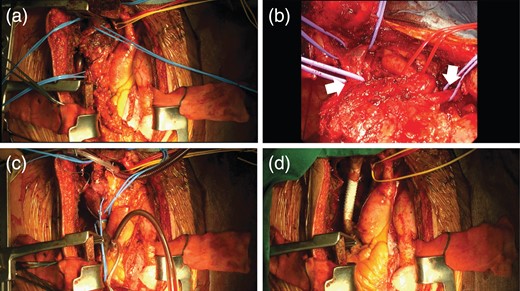
Median full sternotomy with a right TMA was performed to obtain good exposure of infraclavicular region (a). The tumor was invaded to pericardium, right upper lobe of the lung, bilateral brachiocephalic veins (white arrows), azygos vein, right phrenic nerve and SVC (b). Under a temporal veno-venous bypass between right internal jugular vein and right atrial appendage (c), SVC was reconstructed with synthetic vessel (d).
Discussion
Thymic carcinoma is a rare aggressive neoplasm arising from the epithelial cells of the thymus. Because of its rarity, the therapeutic strategy of locally advanced thymic carcinomas has yet to be determined. In National Comprehensive Cancer Network guideline, chemotherapy with or without radiation therapy is recommended as an initial therapeutic option for unresectable or metastatic thymic carcinomas [3], and it would be able to maximize the chance of complete resection of these tumors.
Thymic adenocarcinoma is extraordinarily rare. In our case, the tumor specimen obtained by initial percutaneous biopsy was histologically diagnosed as adenocarcinoma with enteric differentiation, and we had to distinguish primary thymic carcinoma from metastatic disease. Recently, Moser et al. [4] reported two cases of thymic adenocarcinoma with enteric differentiation and proposed that this represented a novel subtype of thymic carcinoma. They also suggested that the knowledge of this subtype will help to avoid misdiagnosis as metastatic disease from an extrathymic primary.
If the thymic tumors invade cervicothoracic great veins such as brachiocephalic veins or SVC, it would often be possible to resect these vessels concomitantly and reconstruct them by using synthetic vessels. Sekine et al. [5] demonstrated their experiences of prosthetic reconstruction of SVC for malignant tumors and concluded that it was feasible. To ensure the quality and safety of operations, it is necessary to select most appropriate approaches when we perform extensive surgery for locally advanced thymic tumors. TMA, which was first reported by Grunenwald and Spaggiari [6], is one of the useful surgical approaches, which may expand the possibility of complete resection of neoplasms involving the thoracic outlet. In general, this approach is suitable for anterior Pancoast tumors; however, it can sometimes be applied practically for various diseases. Di Rienzo et al. [7] reported their experiences of TMA for five different indications and concluded that TMA is a valid technique for the treatment of several kinds of tumors of the cervicothoracic inlet, giving good exposure of the operative field. In our case, we adopted TMA for a case of locally advanced thymic carcinoma invaded the great veins after induction CRT. To our knowledge, there is no literature in which similar cases were reported. We proved that a better surgical field was obtained by TMA for cases of locally advanced thymic carcinoma, allowing safe vascular control and sparing the clavicle. In addition, this approach could give the good post-operative cosmetic and functional outcomes, with no limitation.
References



