-
PDF
- Split View
-
Views
-
Cite
Cite
Oliver C. Bellevue, Bennett M. Johnson, Andrew F. Feczko, Daniel E. Nadig, David M. White, Theatrical fire pursuant exploratory laparotomy, Journal of Surgical Case Reports, Volume 2016, Issue 6, June 2016, rjw100, https://doi.org/10.1093/jscr/rjw100
Close - Share Icon Share
Abstract
Fire in the operating theater is a rare but potentially fatal complication. We report igniting an intraperitoneal fire while preforming an exploratory laparotomy for perforated viscus. Fortunately, the patient suffered no injuries as a result.
Introduction
Fires in the operative theater are rare, but preventable events. They are generally associated with airway surgery or the use of high energy devices such as lasers. Very limited data regarding the ignition of gastrointestinal gas is present in the literature. We report the ignition of an intraperitoneal fire while preforming an exploratory laparotomy for perforated viscus and review other similar reports.
Case Report
A 63-year-old cachectic female with a medical history of multiple myeloma and advanced amyloidosis was admitted to our institution with complaints of left lateral thigh pain and nausea. At the time of presentation, her myeloma and associated vertebral fractures were under active treatment with cyclophosphamide and bortezomib. Ibuprofen had been prescribed 10 days prior to admission for musculoskeletal pain. The patient’s nausea was associated with increasing abdominal distention over approximately 3 months. Computerized axial tomography performed on admission (Fig. 1) demonstrated a dilated stomach containing fecalized material. The patient reported passing gas and stool. She was placed on a general diet and was managed without nasogastric decompression as per her medical team. She continued to receive ibuprofen and was treated with pulse dose steroids, cyclophosphamide and bortezomib until hospital day 5 when the patient complained of sudden, severe abdominal pain.
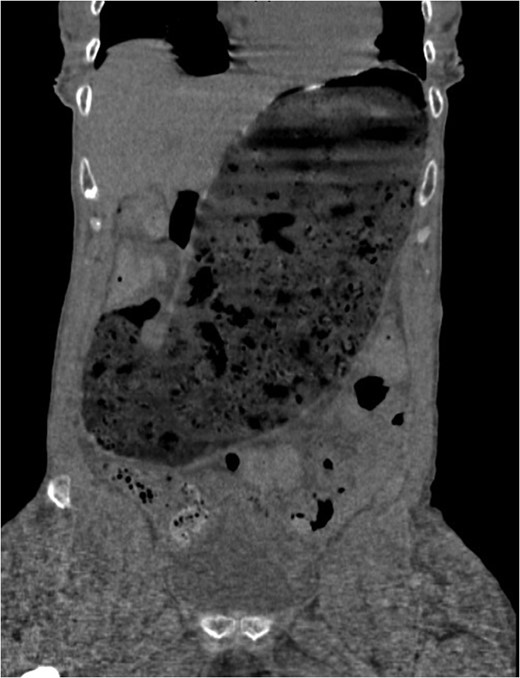
Computed tomography scan at presentation (prior to perforation) demonstrating gastric distention secondary to amyloid provoked gastroparesis with fecalization of gastric contents.
An abdominal plain film revealed substantial pneumoperitoneum and general surgery was consulted with concern for perforated viscus. Examination at that time revealed a tympanic, diffusely tender abdomen without overt signs of peritonitis. The patient’s amyloidosis had resulted in severe macroglossia with multiple episodes of epistaxis and glossal hemorrhage. Nasogastric decompression was deliberately deferred given her friable macroglossia and expected endotracheal intubation. She was taken to the operating theater for exploratory laparotomy which preceded in standard fashion after rapid sequence induction.
Electrocautery was used to dissect through the subcutaneous tissues. When a deliberate incision was made into the peritoneum a loud clap was heard which was followed by a dull roar and 3–4 s of blue flame erupting from the peritoneal cavity. In this interval, the attending physician attempted to extinguish the fire with a moist towel causing a superficial burn to one of his fingers. When the flame had self-extinguished, the patient’s wound was inspected and remarkably found to be free of injury or burn. The abdomen was inspected thoroughly and was also without any evidence of burn injury. An ulcer found on the greater curvature was biopsied and Graham patched. The pylorus was hypertrophic, but widely patent with good movement of gastric contents into the duodenum.
Post-operatively the patient did well without apparent complication. An upper gastrointestinal series was performed on post-operative day 5 (Fig. 2) which was negative for leak but notable for very limited transit of contrast into the duodenum 2 h after administration. Her pathology returned negative for H. Pylori, negative for malignancy, but positive for abundant amyloid deposits. Ultimately, she was discharged home to hospice care given her overall decline.

Upper gastrointestinal series 2 h after gastrograffin contrast administration down nasogastric tube demonstrates no leak and no passage of contrast from severe gastroparesis.
Discussion
The rapid exothermic combustion of gastrointestinal gasses is a rarely described, if feared complication in the operating theater. The American Society of Anesthesiologists endorses the ‘fire triad,’ composed of an oxidizer, an ignition source and a fuel [1]. The principle oxidizers found in the operating room are the oxygen enriched environment and nitrous oxide. Ignition usually occurs secondary to electrocautery, argon beam coagulators, lasers and other sources of electrical current. Fuels include volatile solutions such as alcohol, ether, chlorhexidine, acetone as well as drapes, sponges, blankets, packing materials and gastrointestinal gasses (methane and hydrogen).
Although reportable to the Federal Drug Administration, the number or type of surgical fires per year are not published. The Emergency Care Resource Institute estimates that 200–240 fires occur annually within the United States [2]. Although fires are reported with more frequency in colonoscopy, other authors have witnessed similar gastrointestinal gas ignitions (Table 1).
All reported studies of theatrical fires involving the ignition of gastrointestinal gasses. The heat source in all incidents was electrocautery.
| Author . | Year . | Indication . | Fuel . | Harm . |
|---|---|---|---|---|
| Joyce [3] | 1989 | Decompressive gastrostomy | Gastric gas | Gastric rupture with ignition. |
| Dhebri [4] | 2002 | Gastric perforation | Gastric gas | Rupture of diagram, splenic tears requiring splenectomy and death 3 h post-operative. Flash burn to surgeon’s face with singeing of eyebrows. |
| Mansfield [5] | 2012 | Gastric perforation | Intraperitoneal gas | No harm to patient, 2nd degree burn to surgeon’s finger. |
| Mumith [6] | 2013 | Cecal perforation | Intraperitoneal gas | No harm to patient, partial thickness burn to surgeon’s hand. |
| Raghavan [7] | 2015 | Toxic megacolon | Colonic gas | No harm. |
| Raghavan [7] | 2015 | Transverse colon perforation | Intraperitoneal gas | No harm. |
| Author . | Year . | Indication . | Fuel . | Harm . |
|---|---|---|---|---|
| Joyce [3] | 1989 | Decompressive gastrostomy | Gastric gas | Gastric rupture with ignition. |
| Dhebri [4] | 2002 | Gastric perforation | Gastric gas | Rupture of diagram, splenic tears requiring splenectomy and death 3 h post-operative. Flash burn to surgeon’s face with singeing of eyebrows. |
| Mansfield [5] | 2012 | Gastric perforation | Intraperitoneal gas | No harm to patient, 2nd degree burn to surgeon’s finger. |
| Mumith [6] | 2013 | Cecal perforation | Intraperitoneal gas | No harm to patient, partial thickness burn to surgeon’s hand. |
| Raghavan [7] | 2015 | Toxic megacolon | Colonic gas | No harm. |
| Raghavan [7] | 2015 | Transverse colon perforation | Intraperitoneal gas | No harm. |
All reported studies of theatrical fires involving the ignition of gastrointestinal gasses. The heat source in all incidents was electrocautery.
| Author . | Year . | Indication . | Fuel . | Harm . |
|---|---|---|---|---|
| Joyce [3] | 1989 | Decompressive gastrostomy | Gastric gas | Gastric rupture with ignition. |
| Dhebri [4] | 2002 | Gastric perforation | Gastric gas | Rupture of diagram, splenic tears requiring splenectomy and death 3 h post-operative. Flash burn to surgeon’s face with singeing of eyebrows. |
| Mansfield [5] | 2012 | Gastric perforation | Intraperitoneal gas | No harm to patient, 2nd degree burn to surgeon’s finger. |
| Mumith [6] | 2013 | Cecal perforation | Intraperitoneal gas | No harm to patient, partial thickness burn to surgeon’s hand. |
| Raghavan [7] | 2015 | Toxic megacolon | Colonic gas | No harm. |
| Raghavan [7] | 2015 | Transverse colon perforation | Intraperitoneal gas | No harm. |
| Author . | Year . | Indication . | Fuel . | Harm . |
|---|---|---|---|---|
| Joyce [3] | 1989 | Decompressive gastrostomy | Gastric gas | Gastric rupture with ignition. |
| Dhebri [4] | 2002 | Gastric perforation | Gastric gas | Rupture of diagram, splenic tears requiring splenectomy and death 3 h post-operative. Flash burn to surgeon’s face with singeing of eyebrows. |
| Mansfield [5] | 2012 | Gastric perforation | Intraperitoneal gas | No harm to patient, 2nd degree burn to surgeon’s finger. |
| Mumith [6] | 2013 | Cecal perforation | Intraperitoneal gas | No harm to patient, partial thickness burn to surgeon’s hand. |
| Raghavan [7] | 2015 | Toxic megacolon | Colonic gas | No harm. |
| Raghavan [7] | 2015 | Transverse colon perforation | Intraperitoneal gas | No harm. |
Compared with these other published reports, our patient faired relatively, even surprisingly well after this intraabdominal explosion. We speculate that nasogastric decompression prior to the operating room, deferred given the patient’s friable macroglossia, may have mitigated her intraperitoneal gaseous environment to an extent that may have prevented this fire. Although preoxygenated, she underwent rapid sequence induction and we do not suspect that any significant amount of 100% oxygen was pumped into her peritoneal cavity. Despite not having a mechanical gastric outlet obstruction, amyloid-induced gastroparesis resulted in the optimal environment for fermentation. We strongly recommend sharp entry into the peritoneal cavity whenever intraperitoneal gastrointestinal gasses may be present.
Conflict of interest statement
None declared.
References
https://www.ecri.org/Accident_Investigation/Pages/Surgical-Fire-Prevention.aspx. (14 May 2016, date last accessed).



