-
PDF
- Split View
-
Views
-
Cite
Cite
Efstathios Pavlidis, Ioannis Gkizas, Olga Mavromati, Nikolaos Milonakis, Kahlan Syrianos, Splenic injury following elective colonoscopy: a rare complication, Journal of Surgical Case Reports, Volume 2016, Issue 12, 1 December 2016, rjw214, https://doi.org/10.1093/jscr/rjw214
Close - Share Icon Share
Abstract
Splenic injury is an extremely rare, yet serious, complication related to colonoscopy. So far, less than 80 cases have been reported worldwide since 1970. With the increasing use of colonoscopy, endoscopists, surgeons and radiologists are more likely to encounter this unusual complication. Increased splenocolic adhesions, splenomegaly or underlying splenic disease might, inter alia, constitute a predisposing factor. However, it might also occur in patients without significant adhesions or underlying splenic pathology. Patients with abdominal pain, hypotension and a fall in hematocrit without rectal bleeding after colonoscopy, should be suspected of having splenic injury. Most patients present with symptoms within 24 hours after colonoscopy, nevertheless, delayed presentations have been described as well. We report such a case of splenic injury secondary to colonoscopy. The patient was presented with hemorrhagic shock and abdominal pain following a colonoscopy which had taken place before 36 hours, an urgent splenectomy was required with successful outcome.
INTRODUCTION
Colonoscopy is an excellent diagnostic and therapeutic tool, but not without serious complications. Hemorrhage and perforation of the colon are the most common complications after colonoscopy, occurring in <1% of patients and often associated with biopsy or polypectomy. Many other rare complications have been described such as bacteremia, vasovagal problems, ileus, electrocardiogram abnormalities, mesenteric tears, pneumothorax, pneumoperitoneum, pneumoscrotum and colonic volvulus [1–3].
Splenic injury after colonoscopy is rare, but serious complication of the procedure that may become even a lethal one. The most possible mechanism responsible for causing the complication at hand is tension on the splenocolic ligament or on preexisting adhesions consequent to manipulations into the colon, or as a result of a direct injury to the spleen during passage of colonoscope through the splenic flexure. Intraperitoneal adhesions or any underlying splenic pathology may increase this risk. With the increasing utilization of colonoscopy, both endoscopists and surgeons should be aware of this rare life-threatening complication following this procedure. A case of splenic rupture diagnosed 36 hours after elective colonoscopy that required an emergent splenectomy is reported in this manuscript.
CASE REPORT
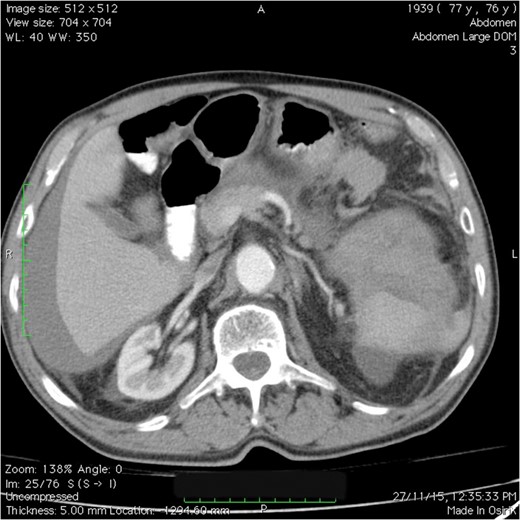
CT scan of the abdomen and pelvis: splenic injury with a large amount of blood in the left upper quadrant, perihepatic region and pelvic areas.
The patient underwent an emergent exploratory laparotomy. It revealed 2500 ml of blood and clots within the peritoneal cavity, integrity without perforation of the colon and a bleeding from the splenocolic ligament and splenic hilum. A splenectomy was performed and a drain was left in place. Surgical specimen histopathology examination showed a rupture spleen with no other underlying pathology. The patient remained stable postoperatively over the course of his hospitalization. The drain was removed on the third postoperative day, when the patient tolerated on oral diet also. He was discharged on the fifth postoperative day with an uneventful postoperative recovery.
DISCUSSION
A review of the literature indicates that the first case of splenic injury associated with colonoscopy was reported in 1974 [4] and less than 80 cases have been reported in the world literature since then [5]. The most likely mechanism responsible for this complication is tension on the splenocolic ligament, or on preexisting adhesions, or on both, due to manipulations of the sigmoid, descending colon or transverse colon or due to a more direct effect, occurring during the passage of the endoscope through the splenic flexure resulting in parenchymal tears or avulsion of the spleen [6]. Splenic rupture can also occur in a normal spleen after a technically demanding colonoscopy. A history of previous abdominal surgery or trauma constitutes a high-risk factor for splenic injury, owing to the fact that splenocolic adhesions may exist. Hematological, infectious and infiltrative diseases that led to splenomegaly, inflammatory bowel disease and pancreatitis increase the risk for splenic rupture after colonoscopy. However, many splenic injuries have been occurred in otherwise reportedly easy colonoscopies in patients without significant adhesions. Other contributing factors to splenic injury include certain techniques used to navigate the splenic flexure, such as the blind advancement of the endoscope past the splenic flexure and hooking the splenic flexure to straighten the left colon [7]. Splenic injury has also been reported in association with colonic perforation after colonoscopy and following endoscopic retrograde cholangiopancreatography in two case reports [8, 9].
The most common signs and symptoms of the aforementioned complication are abdominal pain without radiographic evidence of perforation, left shoulder pain, peritoneal irritation and orthostatic changes. Owing to a low index of suspicion, many of the previously reported cases were diagnosed relatively late even up to 10 days after the procedure.
CT scan is highly accurate for detecting splenic injury and the extent of hemoperitoneum. This examination is considered the diagnostic modality of choice in a stable patient [7]. Although splenectomy is required in the majority of cases, observation or splenorrhaphy may represent alternative options for the surgeon in certain cases. The non-operative approach is usually preferred in patients with no intraperitoneal blood, a closed subcapsular hematoma and a stable hemodynamic status [3].
Three deaths have been reported secondary to splenic rupture after colonoscopy. Two cases occurred during emergent laparotomy, and one case was found during autopsy after the patient's death from severe shock [10]. All other patients had successful outcomes, including those patients undergoing splenectomy and expectant management.
The onset of symptoms usually occurs within the first 24 hours following the procedure. Treatment may include close observation, embolization or splenectomy. In our case, the spleen could not be preserved, and splenectomy was mandatory due to the fact that the injury could not be managed by using conservative techniques.
Splenic injury and rupture are infrequent complications of colonoscopy which must not be forgotten in the differential diagnosis of post-procedural pain. Both endoscopists and surgeons need to suspect splenic injury after colonoscopy in a patient who develops abdominal pain and tenderness without any evidence of bowel perforation or rectal bleeding with or without hemodynamic instability.
CONFLICT OF INTEREST STATEMENT
None declared.



